
Mobile tablet computers equipped with clinical apps for medical image review aren't going to replace diagnostic workstations anytime soon because radiologists still need "real estate" when evaluating subtle images. This was one nugget of advice gleaned by attendees at the recent New York Medical Imaging Informatics Symposium.
Dr. David Hirschorn, director of radiology informatics at Staten Island University Hospital, explained that while mobile devices offer the advantage of viewing radiology images on the fly when a diagnostic workstation is not available, they are limited in functionality.
"When the U.S. Food and Drug Administration [FDA] stated that mobile tablets had new technological characteristics that raised new types of safety and effectiveness questions, the FDA was not simply knee-jerking," Hirschorn said. "Agency officials were rightfully concerned about whether radiologists could make accurate diagnoses."
 Dr. David Hirschorn.
Dr. David Hirschorn.
He explained that the FDA has been approving apps for specific mobile hardware devices to view high-contrast, low-resolution images, specifically CT, MRI, nuclear medicine, and PET scans. These display well when configured on a small display matrix, such as those found on tablet PCs. He noted that a single CT image is relatively tiny, 512 x 512 pixels, a quarter of a megapixel (MP).
"The types of exams that the FDA approved for diagnostic viewing are also high contrast," he said. "It's no surprise that the FDA said it would accept small matrix images for this application."
Radiography images are much larger and tend to be more subtle, which makes it more challenging to view them on a mobile display. A chest x-ray, as an example, is a 5-MP image. Hirschorn pointed out that when looking for a calcification, it isn't possible to sharpen the contrast much because the image might "bloom."
In his opinion, radiologists are most comfortable and efficient when reading a routine chest radiograph displayed on a monitor with a 20 x 24-inch display. "You won't find a radiologist who wants to read a chest x-ray off an Apple iPad. It's not what it's meant for," Hirschorn said. "We generally want visual real estate giving us a lot of space to investigate."
Another drawback for radiologists is that mobile devices are designed for the consumer market. Their displays cannot be calibrated. A tap test has been added to a mobile medical app that will show if there is enough contrast in the image, and if the ambient light is sufficient. When the display screen is tapped, a circle appears; it takes into account the display capabilities of the device, the ambient condition, and the viewer's eyes. The tap test measures the entire imaging chain, and it enables a user to know at that moment in a specific physical location if conditions are good enough to make a diagnosis from the image.
"Only do it right or don't do it at all," Hirschorn added. "When you are being asked to look at one case and render an opinion, mobile devices can be a godsend. It's up to the radiologist to determine if the situation is appropriate."
An update on medical displays
Elizabeth Krupinski, PhD, professor and vice chair of research in radiology at the University of Arizona, has spent most of her professional career working with display monitors. She shared her recommendations about what to consider when purchasing a display monitor for clinical applications.
"There are a lot of technology changes taking place that can affect the way that we choose displays," she said. "Traditional workstation displays will be part of the diagnostic future. You don't want to sit all day long in front of an iPhone or iPad making diagnoses. It's impractical."
New features are emerging, she said, but if they serve absolutely no utility to anyone, then what is the point of purchasing them? It's the quality of the display that allows a radiologist to render a relevant diagnostic decision in an effective and efficient manner.
 Elizabeth Krupinski, PhD.
Elizabeth Krupinski, PhD.
Krupinski defines quality as the accurate and efficient conveyance of information. This includes interpretation efficiency with respect to viewing time spent, level of use of image processing tools and decision aids, and reporting. Diagnostic accuracy involves a variety of factors that are affected by the image display. This includes ease of detection, discrimination or classification, measurement, how accurate the recommended action is from the interpretation, and consistency of making accurate diagnoses.
"The quality of a display will affect all of these factors," she said. "What most studies have concentrated on is detection, and there's much discussion about a display's capability to facilitate detection. I personally think that this is a very small part of the diagnostic process, because most radiologists can detect what's there. However, what they do with a finding after it is detected is affected by the quality of the image and the quality of the display."
Poor displays reduce efficiency. If a monitor is not properly calibrated or if it is not maintaining a minimum luminance of 250 cd/m2, it probably will affect a radiologist's interpretation efficiency because more time may be spent using image processing tools to compensate for the display quality.
"Evaluate new features in displays based on utility," Krupinski suggested. "Maintain a 'buyer beware' attitude."
There's evidence that medical-grade monochrome monitors may no longer be needed; they can be replaced by high-quality off-the-shelf commercial color monitors that incorporate calibration capabilities. The new generation of high-quality monitors with in-plane switching (IPS), in which crystal molecules move parallel to a panel plane instead of perpendicular, reduces light scatter and noise.
High-performance displays of 30 inches or larger can be useful, depending on how they are used. Because they are larger, they display larger images. This feature may or may not be needed.
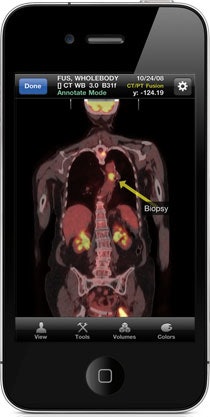 The FDA in 2011 cleared Mobile MIM, the first app for reviewing medical images on iPhone and iPad devices. Image courtesy of MIM Software.
The FDA in 2011 cleared Mobile MIM, the first app for reviewing medical images on iPhone and iPad devices. Image courtesy of MIM Software.
Ten megapixel (4096 x 2560 pixels) monitors are now commercially available. Do radiologists need them? Multiple studies have confirmed that 5-MP monitors display enough detail for mammography exams, but no clinical studies have been published to determine if 10-MP monitors are better. These might be useful for digital pathology image viewing, Krupinski suggested, but she is not yet convinced they will help radiologists.
There is one exception, however. Larger 10-MP displays might allow a lot of people to have a diagnostic viewing experience, and they can be useful for clinical conferences and grand rounds because they enable viewers to perceive subtle findings better.
The standard recommendation that a monitor with eight bit levels is sufficient compared to 11-bit monitors still holds. Krupinski described a study she and her colleagues conducted that measured radiologists' performance when using a workstation with an 8-bit monitor and one with an 11-bit monitor. There were several second performance differences with the 11-bit monitor, but from a daily workload perspective, the impact was negligible.
What is exciting is that today's monitors are packed with smart and automated functions. Monitors are equipped with backlight sensors detecting luminance, and they may have temperature and ambient light sensors as well. They may automatically correct to maintain luminance, performed either by online monitoring or by manual activation working in the background.
"These are excellent tools because radiologists want a monitor that is calibrated and maintains a uniform display on a daily basis," Krupinski said. By having stable and efficient performance, the monitor is more consistent over time, and its useful lifetime is extended.
Krupinski pointed out that there are trade-offs between automation and how much control a user has. She thinks that automation relating to calibration is appropriate and useful, especially for radiologists working in a private-practice setting who don't have a medical physicist to tweak the monitors on a daily basis, or the expensive tools needed for calibration.
"Some degree of automation takes the burden of constantly monitoring the quality of the display and puts it on the manufacturer," she said. "This is a job that a vendor should be doing."
As for protective coatings, get them if you are the type of person who smudges a display with fingerprints, she suggested. If radiologists don't touch the display, protective coatings are not worth the extra cost. Antiglare and reflection coatings, which were necessary for cathode ray displays, are not needed for LCD displays because reflection is no longer an issue.
With respect to the performance of a high-quality commercial color monitor versus a medical-grade color monitor, it has been nearly identical since 2009, Krupinski said. Commercial systems should, however, have calibration features.
Stereoscopic and 3D displays are evolving, but they are still in an experimental phase for clinical applications. Future systems with automatic eye-tracking capability and intelligent software may provide navigation assistance. Krupinski said she looks forward to their evolution.
But in dealing with the present, it's important to recognize that there is a trade-off between display performance and cost. Purchase what will help improve the diagnostic process, she advised.



















