Researchers in Boston have developed an automated radiation-exposure monitoring system that extracts detailed CT exposure data from image repositories. Thanks to optical character recognition (OCR) software, the open-source software scheme can gather data from virtually any CT scanner model, even older ones without DICOM-based dose displays.
In a sample of 54,549 CT encounters over the past decade, the modified open-source toolkit achieved nearly 100% accuracy in data capture, according to a presentation at the recent RSNA 2011 meeting.
Dose monitoring has become a hot topic thanks to CT's explosive growth over the past decade, leading to efforts to optimize radiation exposure in routine clinical practice. Despite this work, some scanning protocols remain widely variable within and across institutions, leading to higher-than-necessary radiation doses that can potentially harm patients, said Maj. Graham Warden, MD, from the U.S. Air Force Medical Corps, in his RSNA talk.
Among the many challenges in radiation dose monitoring and archiving, anatomy-specific CT exposure metrics need to be extracted from existing image repositories, stored, and organized in databases that can be accessed by multiple institutions, Warden said. Warden's study, performed at Brigham and Women's Hospital and several other regional medical centers, aimed to validate the performance of an open-source tool that automatically extracts this information, and it shows how the resulting data can enhance radiation monitoring efforts.
"Most scanners aren't able to produce the new DICOM structured dose reports," said Warden, who led the dose-capture research as a resident at Brigham and Women's. Instead, most available dose information is contained in CT dose report screens with condensed study-level reports, and in dose event-specific data in formats that vary by scanner model and vendor.
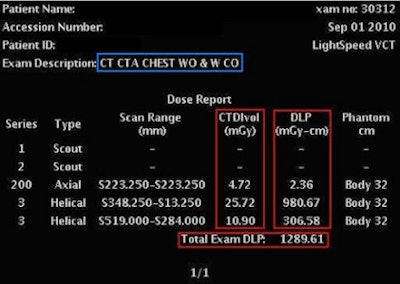 |
| CT dose report screens can vary widely between vendors and scanner models, but an intelligent retrieval system combined with optical character recognition can be used to aggregate data from different displays. All images courtesy of Maj. Graham Warden, MD. |
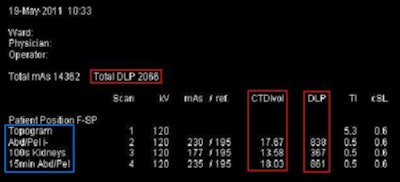 |
Large-scale dose data are needed now, Warden said, to improve awareness of dose information, as well as to validate and refine models of the biological effects of dose exposures. To do this, institutions need to accumulate "large-scale, actionable" dose data, which can be done with open-source software and optical character recognition software.
Dose information from newer CT scanners is based on the 2007 DICOM CT Radiation Dose Structured Report (RDSR) standard for encoding CT dose, as well as the Integrating the Healthcare Enterprise (IHE) Radiation Exposure Monitoring (REM) profile standard framework encompassing dose report generation, management, and submission for dose registries, he said.
But for now, the vast trove of available dose information comes in so many different formats that it can't be aggregated without a nimble system able to recognize them all. That's where open-source and OCR software come in, he said.
Warden, Dr. David Clunie, and colleagues developed software that extracts anatomy-specific CT exposure data through OCR dose report screen captures, in combination with DICOM attributes, he explained.
The software tool was derived from Clunie's PixelMed Java open-source DICOM toolkit, which supports the DICOM operations C-FIND and C-MOVE. PixelMed identifies and retrieves images directly from the DICOM archive, Warden said. The resulting application has the following capabilities:
- Uses OCR to convert CT dose screens to text using glyph matching
- Uses regular expressions to parse text and extract dose information in different formats
- Uses DICOM header information to construct dose information
- Adds DICOM CT RDSR dose and anatomy classes that define anatomic regions using Systematized Nomenclature of Medicine (SNOMED) terminology
- Provides support for dose screens produced by GE Healthcare and Philips Healthcare
To this, the researchers added support for formats from Siemens Healthcare and Toshiba America Medical Systems, and improved the anatomy-extraction capabilities in a variety of ways. In addition, automated batch processing was added to the application to enable it to run on a large scale and to create the database. The extended toolkit that emerged from these modifications is known as General Radiation Observation Kit (GROK).
Testing the tool
To test the software, Warden's group used a cohort of about 54,500 CT encounters randomly selected between 2000 and 2010, utilizing the new software tool to extract the data. From that cohort, they looked at a random selection of 150 CT dose report screens from each of the four CT manufacturers, Warden said. All of the dose information was automatically populated in the database by the extraction tool.
The researchers then measured the recall of dose report screen captures and the extraction precision of the exposure metrics, as well as the accuracy of the automated anatomy assignment of each dose report captured by the software tool.
The results of the data-capture test showed that 55% (29,948 of 54,549) of the CT encounters had at least one detected dose screen. They found that the prevalence of dose screens on scanners rose from 10% (22 of 216) in 2002 to 95% (1,857 of 1,956) in 2010 -- "basically because we changed our PACS and didn't fully migrate the images over" to the new network, he said. In addition, the facility underwent a major scanner upgrade in 2005 and 2006.
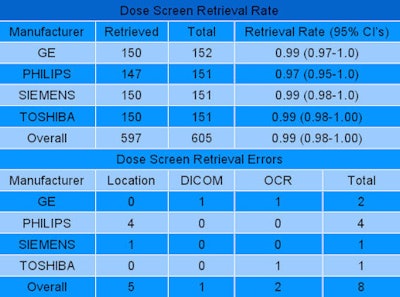 |
| The dose screen retrieval rate approached 100% for all vendors and scanner models. |
The toolkit is fast, Warden said, and is able to extract about 500 CT exams per hour. More than 90% of the extraction time is taken up by image transfer, Warden added. The dose screen retrieval rate was 99%.
"It's easier with some vendors because they put [dose screens] in a reliable location," he said. "The few that we weren't able to retrieve were due to it not being in the expected spot, the DICOM image attributes not being of the expected values, or occasionally unrecognized characters with OCR."
Assigning anatomy to images, where overall assignment precision reached 94%, took time to address because the information is found in different places on different scanners and naming isn't standardized, Warden said. Extracted dose-length product (DLP) and CT dose index volume (CTDIvol) information were always correct, he said, but errors crept in with regard to naming (inadequate or inaccurate study, series, or protocol descriptions), matching (useful anatomic information present in image-level DICOM attributes but not matched to corresponding dose event), and OCR.
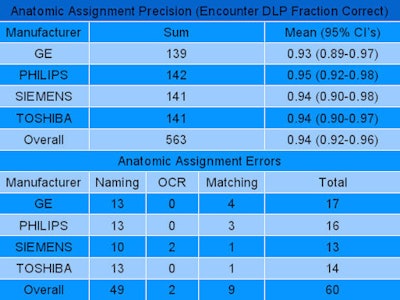 |
| Analysis of more than 54,000 cases demonstrated overall anatomic assignment precision of 94%. Extracted DLP and CTDIvol were 100% correct, but anatomic errors were found in naming, matching, and occasional unrecognized characters. |
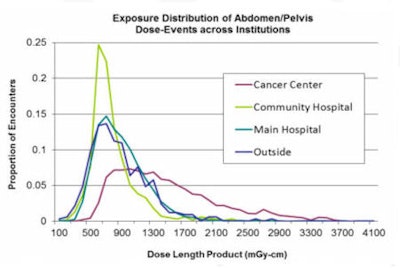
There are several ways to use the data, Warden said. For example, automated anatomic assignment allows comparison across institutions despite widely variable procedure descriptions. The system can also help identify potentially inappropriate variation, along with protocol standardization and optimization targets.
"You can take all of your protocols on the same scanner, on different scanners, and then look for protocols that might be outliers," Warden said. "You can use the same data to refine your cumulative estimates of patient dose, with the big caveat being that to really do this right you need better patient characteristics, the hardest of which is body habitus. You need age, gender, and body habitus, at minimum."
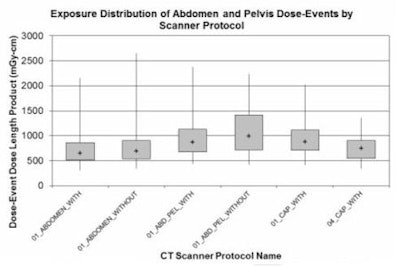 |
| Comparing doses by scanner protocol may help identify potentially inappropriate variations in dose, as well as identify protocol standardization and optimization targets. |
Large-scale extraction of exposure data from image archives is possible, with relatively high retrieval and precision despite the heterogeneity of the anatomic descriptions, Warden concluded.
"We can use the information to enhance quality and safety at multiple different levels, but to go further in this we need better methodology to better estimate body habitus," he said. "Some of the ongoing work we're doing with the same project is to automatically at the dose-event level look at the patient's body habitus at the exposure event."
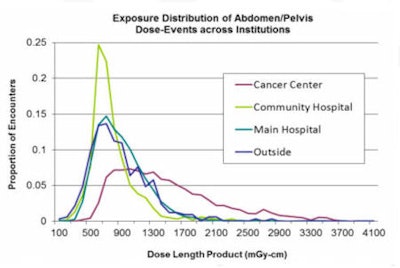 |
| Automated anatomic assignment allows comparison across institutions despite widely variable procedure descriptions. |
One relatively simple way to do this is to check the attenuation of the image, assign that attenuation to the patient, and model the image attenuation of the patient as one would a cylinder of water. This technique provides an effective diameter for the patient, and size-specific dose estimates can be used to refine the resulting dose calculations, he said.
For combined acquisitions such as chest, abdomen, and pelvis scans, measuring scan length can help discern the covered anatomy and, with a little additional work, even break the images down into their component parts for archiving and comparison to other scans, Warden said.



















