CHICAGO - RSNA's Image Share pilot program for patient-driven image exchange has encountered a small number of problems with participants, but most are technical or IT-related and can be readily solved, according to research presented on Sunday at the 2012 RSNA meeting.
While the number of overall reported patient problems remains low, analysis of the issues encountered by the program's help desk revealed that most were related to technical and IT matters, rather than problems with the software used in the program. Many of these issues stemmed from growing pains with the personal health record (PHR) vendors participating in the project, the researchers reported.
"There haven't been too many issues that can't really be resolved [from] a technical aspect," said presenter Dr. Yousaf Awan, of the University of Maryland, during the Sunday morning scientific session.
The current method of image sharing between healthcare institutions has a number of limitations, Awan said. CDs are often incompatible with specific PACS software, and CD image viewers can be low-quality.
"These shortcomings often lead to repeat imaging and increased radiation exposure for patients when they don't necessarily need them," he said.
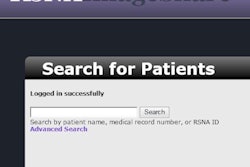
To tackle this problem, RSNA undertook a pilot program to provide efficient image sharing. With Image Share, images are pushed to an online server, and they can be accessed at any time and any place where Internet access is available. Each exam also has a secure token/ID and password associated with it, Awan said.
Under the Image Share system workflow, images are processed by a clearinghouse before going to the PHR. The University of Maryland was instrumental in developing the software that pushes the images to the clearinghouse, Awan said.
Healthcare institutions currently participating in Image Share include the University of Maryland Medical Center; the Mayo Clinic in Rochester, MN; the University of California, San Francisco; the University of Chicago; and Mount Sinai Medical Center.
The project aims to produce a paradigm shift away from the traditional flow of imaging in which patients have been uninvolved, he said.
"There has been a major push toward patient-centered healthcare throughout all aspects of healthcare," Awan said. "So the question is: Why can't we extend that push toward the radiology aspect of this? Patients should be at the center of the imaging aspect as well."
As of November 1, there were 2,100 total patients enrolled in Image Share. Of these, 30% to 40% have actually turned on the image sharing capability, said Dr. David Mendelson, chief clinical investigator for Image Share and chief of clinical informatics at Mount Sinai Medical Center.
Patient-centered radiology
Image Share empowers patients regarding their imaging, allowing them to view their imaging at any time, he said. Patients can provide any healthcare provider with their imaging instantly when needed.
Patients participate voluntarily in the project and choose from one of two personal health record applications (Dell or LifeImage) available in the program.
To field any issues experienced throughout the program, a help desk was created and is operated by the University of Maryland. A toll-free number is provided for participants. Issues were tracked using the Mantis free Web-based issue tracking system.
From the thousands of participants enrolled in the program, 211 issues were reported from September 2011 to September 2012, Awan said. The most commonly reported issues encountered by the help desk were patient-specific issues, followed by PHR issues related to either vendor (Dell or LifeImage).
There were six patient-specific issue subcategories: patients were unable to access images; they needed to request to upload new exams; general miscellaneous issues; request for program information; password/ID issues; and to a 72-hour timing issue. The program was initially set up to lock out patients from their exams if they hadn't logged in within 72 hours of receiving their password and token, he explained.
Lessons learned
Anecdotally, patients reported concern with the time it took to resolve issues, Awan said. There was also confusion over the roles of the help desk, enrolling site, and PHR vendor, as well as confusion over the whole program in general, he said.
There were two main subcategories of PHR issues: patients couldn't access images through the PHR, and patients couldn't access their account through the PHR (patient is locked out of the account).
"Many of the issues resolved around initial growing pains with the PHR vendors," he said.
In terms of improving the efficiency of the help desk, the researchers realized that it would be helpful to have more in-depth education and instruction to better inform patients.
"This can begin at the site level and be distributed accordingly," he said.
In addition, each site and PHR vendor need to provide current contacts and hours of operation, Awan added.
"Also, to confirm issue responses and resolution target times from the PHRs, low-level administrative access to PHRs should be made available to expedite small issues such as patients being locked out of their account or resetting a password," he said.
Patient-centered radiology provides a number of advantages, including fewer lost or unnecessarily duplicated studies. Patients can also keep a more consistent and coherent record of their imaging experience. In addition, patients can provide their studies more reliably to referring physicians, Awan said.
This pilot program details the concerns that need to be addressed to further involve patients in their care and imaging and addresses how to resolve them, he said.
"It provides an informational blueprint for those who hope to implement similar programs at their institutions," Awan said.