Part 1 of our series on the Eugene P. Pendergrass New Horizons Lectures at the 2012 RSNA meeting provides coverage of a presentation by Dr. Keith Dreyer, PhD, on the future of radiology informatics. Part 2, covering Dr. Paul Chang's lecture on how medical imaging IT can ensure that radiologists thrive in the new era of healthcare, will be available Wednesday.
CHICAGO - Although healthcare reform and alternatives to the traditional fee-for-service model pose challenges to radiology, advances in information technology can help radiologists clearly demonstrate their value in patient care, according to Dr. Keith Dreyer, PhD, of Massachusetts General Hospital (MGH).
While radiology informatics has dramatically increased radiologist productivity and profitability over the past 15 to 20 years, it has pushed down radiologists' relevance or presence in care, according to Dreyer, vice chair of radiology at MGH. But because of the U.S. government's healthcare IT stimulus program and healthcare reform, image sharing, structured reporting, new communication technology, clinical decision support, electronic health records (EHRs), and personal health records (PHRs) will have a broader impact in the future.
 Dr. Keith Dreyer, PhD, of Massachusetts General Hospital.
Dr. Keith Dreyer, PhD, of Massachusetts General Hospital.
"At the expense of some productivity, we're going see a dramatic increase in quality that will be measurable by metrics that we'll be required to measure but also an increase in relevance," he said.
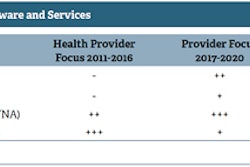
Current radiology business models have been determined by payment models over the past decades, with fee-for-service plans that incentivize volume while being neutral on value. In turn, these business models have determined innovation in radiology, with a focus on maximizing productivity and volume and reducing the cost of doing business, Dreyer said.
"They really haven't been optimized for performance metrics such as quality, safety, access, and outcomes," he said.
If radiologists were incentivized by outcomes, they would likely want, for example, to open up a chat session with referring clinicians who have questions on a difficult case they recently read to guide them through it. If the motive was patients first, they might wish to have a system that extended that chat functionality to patients, Dreyer said.
Teleradiology
Teleradiology created secure access for remote radiologists, but it did not provide secure access for regional colleagues who may be competitors in a fee-for-service model but need to see prior images for their patients, Dreyer said. Furthermore, teleradiology images have not been made accessible to patients; in many cases, they get a CD while radiologists have the luxury of moving images around electronically.
Initially created to improve radiologist productivity and convenience, teleradiology serves to further reduce costs due to economies of scale and geoeconomic shifting.
"The unintended consequence [however] is the potential to serve as a conduit for commoditization of our services," Dreyer said.
With healthcare representing 17% of the U.S. gross domestic product, cost is a primary concern for healthcare reform. Indeed, the U.S. Centers for Medicare and Medicaid Services (CMS) is exploring alternatives to fee-for-service systems such as bundled payments and the use of accountable care organizations, Dreyer said.
These alternatives will shift risk from payors to providers and extends the risk to service lines such as imaging. The burden in this new model will be to monitor and report metrics such as quality, safety, and access before payment can be received for those patients, he said.
This dynamic is embodied in the CMS incentive program for meaningful use to promote the use of certified electronic health record technology (CEHRT). The fundamental goals of the meaningful use program are to improve quality, safety, and efficiency; engage patients and families; improve care coordination; improve public and population health; and ensure privacy and security, Dreyer said.
He highlighted two specific provisions in stage 2 of meaningful use, which will take effect in 2014 and beyond. Ordering physicians must use CEHRT to order more than 30% of imaging exams and to receive more than 10% of imaging results, including the images.
"If we have a disparate physician facility with their own CEHRT and they are using us as an imaging provider, we have to be able to receive their order from their CEHRT, and when we generate an image, we have to be able to make that image available in a link inside of their CEHRT," Dreyer said. "[That's] a little different from what we're doing today. This may be available in our hospitals, but now we need to extend it to those other physicians. ... We have a couple of years to solve this, but it will probably be something like cloud-based image sharing."
Innovation opportunities
With the changes facing radiology, the specialty has three opportunities for innovation, relating to access, communication, and utilization, according to Dreyer.
In the access domain, imaging information is currently too compartmentalized and inaccessible. This may pave the way for the convergence of a lot of RIS and electronic EHR functionality related to enterprise tasks such as ordering, scheduling, and communication, Dreyer said. Departmental RIS functionality will likely converge into PACS, making that a smarter and smarter system.
That doesn't solve the problem of sharing information, however, so image sharing technology will likely be an area of focus in the next few years. If PACS is going to evolve into the imaging health record, it doesn't make sense to have separate systems for inside and outside the institution that perform similar functions, Dreyer said.
For example, he cited the potential of RSNA's Image Share project to support image sharing across facilities.
"The old adage of having RIS and PACS being in a confined area is really going to give away to this kind of new approach," he said. "There's a lot of opportunity for innovation there, clearly."
In the communication domain, radiology reporting today is largely unstructured, unmanaged, and unidirectional, according to Dreyer. This is a quality, safety, and relevance concern.
Innovations to solve this problem could include optimized structured reporting, as well as multimedia, interactive communications.
For structure, "I think of BI-RADS for the rest of radiology, if you will, with actionable findings and actionable recommendations," he said. "One of the quick things that this provides, which we'll need to do for meaningful use, is have radiologists' clinical decision support. So at the time of interpretation, while I'm looking at images and dictating, information can come up as I'm talking, understanding what I'm saying and offering advice for my findings and, mainly, for my recommendations."
Dreyer also emphasized the potential for interactive multimedia communication, such as an internally developed application at MGH that provides mobile access to EHR data and image data. A recent pilot project explored the possibility of offering collaborative opportunities on any device to those physicians who might have a question on a case.
As for utilization, payors today tend to regulate the use of imaging via precertification and preauthorization, which makes it difficult for radiologists to engage and participate in the appropriate ordering of exams. This opens the door for clinical decision support for imaging to provide tools to assist the radiologists and the ordering clinician in utilization management, Dreyer said.
This would include incorporating national imaging guidelines such as the American College of Radiology's (ACR) Appropriateness Criteria. The organization's ACR Select product allows integration of that information directly into CEHRT, Dreyer said.
"Enter the Appropriateness Criteria and a more elaborate interface that allows that connectivity and context of the ordering exam inside the EHR, and what you wind up with is three-way communication between the ordering physician, the dynamic information that's nationally transparent and continuously updated, and the consulting radiologist integrated into that certified health record technology," he said.