Can physician scientists make biomedical research more efficient? Episode 11 of the Keeping Up with the Radiologists podcast tackles that question.
In this podcast, hosts Saurabh Jha, MD, and Mitch Schnall, MD, PhD, talk with Terence Gade, MD, PhD, a physician-scientist engaged in radiology and medical imaging research at the University of Pennsylvania Perelman School of Medicine.
Gade's Penn Image-Guided Interventions (PIGI) Lab has been involved in translational research for the development of novel imaging approaches and advanced therapeutics in interventional radiology. There, Gade emphasizes a team science approach. The convergence of image-guided interventions, cancer/vascular biology, and molecular imaging drive the work.
"The value of translational science is being increasingly recognized," Gade explained during the episode, pointing to the Institute for Translational Medicine and Therapeutics (ITMAT) at the University of Pennsylvania. ITMAT includes investigators from all schools at UPenn, the Children's Hospital of Philadelphia, and the Wistar Institute. Using dry and wet lab research space, ITMAT's projects cross the pediatric-to-adult divide, according to information on the institute's website.
Clinician scientists at Penn Medicine are credited with advances in chimeric antigen receptor (CAR)-T cell therapy, messenger ribonucleic acid (mRNA) vaccines, and understanding beta-amyloid plaques in Alzheimer's disease, Schnall said. Rather than a discussion of these or other academic research projects, the conversation takes us into the perspective of a physician-scientist, what it is, and why it is important.
Key question: how does a physician-scientist versus a nonphysician scientist contribute to biomedical research and play a powerful role in resolving clinical deficiencies?
"There are insights clinician-scientists have that scientists who do not practice medicine would be hard-pressed to have," Schnall explained to tip off the discussion.
Key point: knowledge gained from the medical residency is critical, according to Gade, who reflected on wanting to forego his medical residency -- at first -- but decided against it only to realize the true value of the experience in his translational research work.
"When I was in medical school, translational research wasn't something that was encouraged," Gade said. "Clinical research wasn't necessarily something that was encouraged. They wanted to make sure you would become a scientist [who] was at the level of other PhD scientists. Now, I think more and more we're seeing MD PhDs being trained in translational science, in clinical science, and that being encouraged."
It's a matter of direct clinical impact, according to Schnall, who as many AuntMinnie readers already know is a Penn Medicine physician and diagnostic radiologist, professor of radiology, and senior vice president of data and technology solutions.
"If you look at the history of radiology with both CT and MR, the actual initiation, the discoveries weren't by physicians," added Jha, but the implementation, the scaling was by physicians. "You have physician, scientist, and entrepreneur. If you have all three, that's the 'golden cup.'"
"Someone who can be in the realm of science and in the realm of the clinic enhances that efficiency [for the] translation," Gade added. "Many great ideas never made it into the clinic for no other reason than they just weren't consistent with clinical workflows, really understanding how the clinic works, and how you can actuate these ideas and make them relevant."
Chances of knowing correctly that research is clinically relevant are greater if you have a physician at the helm, Jha emphasized.
During this episode, the panel also discusses developing relevant imaging strategies that address clinical deficiencies, the incorporation of radiochemistry and nuclear medicine in radiology, and where we are with spatial resolution in molecular imaging.
"Insights have dramatically increased in our understanding of biology," Schnall said. "Particularly in the cancer realm using radioimmunotherapy, it's been suggested that, and most radiologists will probably bristle at this, in the next 10 years that's going to be a bigger business than the total imaging technology business put together."
Key question: what are the limits of what we can see with fine molecular imaging?
Key point: it depends on the agent.
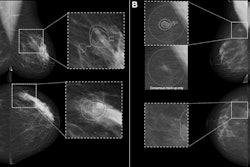
"There are now multiple approaches," Schnall explained. "A lot of people think of molecular imaging and PET as synergistic and that's far from true, although the majority of molecular imaging we do is on a PET scanner in the clinic these days because the chemistry is understood and the technology is well poised, and even PET scanners are getting better every day. The resolution is improving tremendously to the extent that some modern PET scanners almost start to look like old CT scanners in terms of resolution."
Listen as Gade elaborates on the "next realm" of molecular imaging strategies. He also accounts an experience in trans arterial embolization that involved a "fascinating phenomenon" and clinical deficiency. Further, he discusses an imaging modality that involves imaging a fundamental change in glycolysis and not only identifies latent disease that will eventually have an impact on the patient's outcomes but also inspires thinking about how to target it.
Hear more about this (hyperpolarized MRI)-guided precision medicine, its potential therapeutic translation, and more in this episode of Keeping Up With The Radiologists.
More impressions
{01:17:07} Physician / clinician scientists
{06:36:08} Notable clinician scientist achievements
{09:07:24} Clinically relevant or dead
{10:33:19} Addressing relevant clinical deficiencies
{22:29:08} Clinical trial using hyperpolarized MRI
{24:20:28} Steps to scaling, reimbursement, incentives
{26:21:22} Scanner capabilities
{27:43:11} Parametric maps as data
{29:36:22} Adoption, the workflow issue
{31:14:09} Domain of interventional radiology
{34:31:21} Radiology spans all medicine
{36:10:19} Clinician / physician scientist skills approaches
{39:57:27} Focused research programs
{42:07:08} How much science, how much clinic
Guest
Terence Gade, MD, PhD, is associate professor of radiology and cancer biology at the University of Pennsylvania Perelman School of Medicine.
Hosts
Saurabh (Harry) Jha, MD, is an associate professor of radiology at the Hospital of the University of Pennsylvania. Jha obtained a master’s degree in health policy research from the Leonard Davis Institute at the University of Pennsylvania. He earned his medical degree from the United Medical and Dental Schools of Guy’s, King’s, and St. Thomas’ Hospitals. Jha developed Value of Imaging, a set of radiology educational resources.
Mitchell Schnall, MD, PhD, is a physician at Penn Medicine in its abdominal imaging services program. Schnall served as chair of the department of radiology and the Eugene P. Pendergrass Professor of Radiology at the Perelman School of Medicine, before taking on the role of senior vice president for data and technology solutions for the University of Pennsylvania Health System in 2024. Schnall still serves as group co-chair of the ECOG-ACRIN Cancer Research Group since its founding in 2012. He is an international leader in translational biomedical and imaging research, working throughout his career across the interface between basic imaging science and clinical medicine to ensure effective integration of radiology research with other medical disciplines.
This episode of Keeping Up With the Radiologists is brought to you by AuntMinnie.com in collaboration with Penn Radiology. The series is also available on Spotify, YouTube Music, and Apple Podcasts. Check back for new episodes!