
There are so many critical topics of interest in health policy that it is easy for us to overlook Medicaid; however, in this brief I will hopefully give you a summary of where the program stands and where it is going (I have drawn heavily from a June 2005 Issue Paper by the Kaiser Family Foundation, Kaiser Commission on Medicaid and the Uninsured).
Remember that Medicaid is the safety-net program for low-income, uninsured Americans. It is a federal-state program that currently insures 52 million people in one way or another. Some of these are dually eligible for the Medicare program, which offers additional benefits (such as long-term care) to low-income beneficiaries.
In general, Medicaid offers benefits to three major low-income groups: children and their parents, the elderly, and people with disabilities. Populations that receive traditional welfare benefits (cash assistance, temporary assistance to needy families) typically receive mandatory coverage under Medicaid law. Other populations who typically receive these benefits -- and may not receive cash assistance, but are otherwise impoverished -- are now also eligible for Medicaid. Figure 1 gives a summary breakdown of Medicaid beneficiary groups.
 |
The Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (also known as PRWORA or "Welfare Reform") severed the historical link between Medicaid and cash assistance, and furthered the evolution of Medicaid into a health insurance and long-term care financing program rather than a welfare program. Ultimately, the term "mandatory" reflects this history, referring generally to groups traditionally eligible for cash assistance prior to PRWORA.
Those designated under optional populations are low-income individuals who were not necessarily eligible prior to PRWORA. The federal government has "mandated" coverage of mandatory populations and does provide federal matching funds for the "optional" populations.
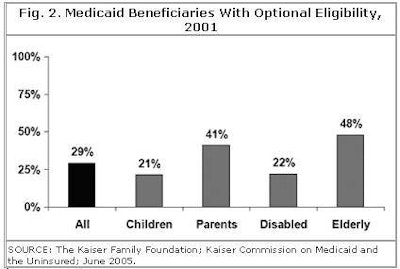
Overall, 29% of Medicaid's beneficiaries qualify on the basis of an optional eligibility group. Figure 2 demonstrates the great variation in categorization by group. Note that nearly half of all elderly persons on Medicaid are eligible under optional categorization.
 |
Medicaid beneficiaries are all entitled to certain mandatory services, such as physician services, hospital care, nursing facility care, and laboratory testing, including the technical and professional components of radiology. It should be noted, however, that Medicaid does not make any promises as to reimbursement levels.
Services offered at the state option include prescription drugs and a broad array of disability-related services such as case management, rehabilitative services, personal care services, and home and community-based services. Many of these optional benefits provide benefits for both the mandatory and optional populations, and are particularly important to the elderly and disabled populations. Figure 3 shows some of the services that are categorized as mandatory and optional for acute care benefits.
 |
If a state decides to extend Medicaid coverage to an optional population, it must generally offer the same benefits package that it makes available to its mandatory populations. In every state, this benefits package includes both mandatory and optional services.
Figure 4 shows the four categories of spending. Please note that mandatory services for mandatory groups make up about 40% of the total. In other words, if states became desperate, they could legally curtail Medicaid by 60%, limiting services and coverage to many marginal populations.
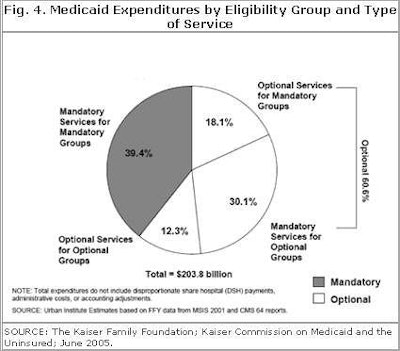 |
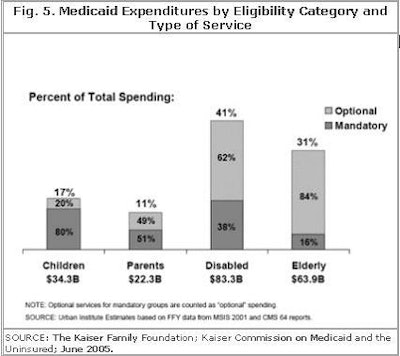
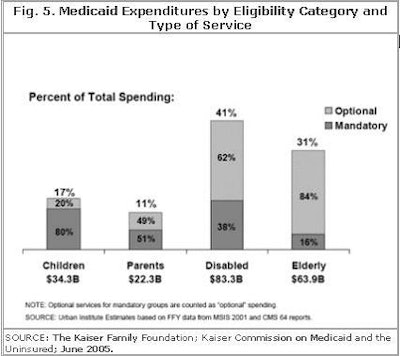
Figure 5 depicts the breakdown of expenditures by eligibility category and type of service. A majority of the services provided to the disabled and elderly are optional services.
 |
Why do all these figures matter to a radiologist or even the average U.S. citizen? The program is enormously expensive at a time when the federal government is running a huge budget deficit, and state government budgets are dangerously out of balance.
State governments pay 43% of Medicaid costs, so it is a major expenditure for the states, complicated by the fact that nearly all states have balanced-budget laws in effect. Daily we see press reports of efforts to rein in the spiraling costs of Medicaid. As radiologists, we know that our services cannot be removed from Medicaid, but what we must remember is that many of our Medicaid-eligible patients are eligible optionally.
Thus, efforts to curtail this necessary program may translate into cuts to the optional populations, leading to a greater number of "self-pay" uninsured patients coming to our practices, particularly if we are hospital-based. Every state is currently looking at ways to reduce optional populations and optional services.
We, as imaging specialists, are in the conflicting position of being a mandated service, while other necessary healthcare services are in danger of being cut. If Medicaid were limited to fewer people and fewer services, we might get better reimbursement. On the other hand, the social consequences of such a change are great and would only lead to a greater uninsured problem in the U.S.
I urge you to see Medicaid for what it is: a true healthcare safety net for the most vulnerable and sick in our midst. Thus, while it may make financial sense to look to Medicaid to save money in tight times, we should remember that this population is least able to help themselves. As physicians dedicated to helping all of our patients, we must recognize that these most fragile groups should be sheltered and protected as well.
By Dr. Howard P. Forman
AuntMinnie.com contributing writer
September 13, 2005
Dr. Forman is an associate editor of health policy for the American Roentgen Ray Society (ARRS). This article originally appeared in the American Journal of Roentgenology (August 2005, Vol. 185:2). Reprinted by permission of the ARRS.
Related Reading
MedPAC, Medicare, and imaging growth, August 16, 2005
Medicare's condition in 2005: critical, June 15, 2005
Health benefits at work: what to expect in the future, May 24, 2005
National health expenditures and another year of 'unsustainable growth', May 4, 2005
ACR criteria cut imaging costs in Israel, January 11, 2005
Copyright © 2005 American Roentgen Ray Society