Is infrared thermography a legitimate adjunctive breast imaging technique, or a clinically questionable technology open to abuse? That's the question being raised following the case of an Oregon clinic that was shut down by state regulatory authorities for offering infrared thermography for breast cancer screening.
The Oregon Department of Justice (DOJ) in April shut down a health clinic in Medford that it claims misrepresented the efficacy of infrared thermography as a breast cancer detection procedure to patients and insurers. The agency also ordered the operators of Laser and Thermal Imaging Center to pay $20,000 in restitution and to warn women who received thermographic imaging at the clinic to get mammograms rather than rely on the facility's thermography testing.
The DOJ's complaint charged that Laser and Thermal Imaging Center owners Mary Anne Crandall, her husband, Thomas Crandall, and her brother-in-law, James Crandall, claimed that thermography could detect the presence of breast cancer seven to 10 years before other diagnostic procedures, including mammography, despite the fact that "medical studies have repudiated thermography as a standalone breast cancer detector," the DOJ said.
The Crandalls were also charged with fraudulent billing practices by charging patients up front for the thermography procedures, promising that insurance companies would reimburse, and then altering billing codes to secure insurance payment that the agency said was "unwarranted."
Mary Anne Crandall also falsely claimed to be licensed as an R.N., a chiropractor, an M.D., and a naturopath, the DOJ said. Neither she, her husband, nor her brother-in-law could be reached for comment.
In addition to the restitution and warning, the settlement between the Oregon DOJ and the center requires the Crandalls to close the clinic and never provide thermography or laser services or present themselves as healthcare providers unless licensed by the state.
"Putting the lives of women at risk is unconscionable," Oregon Attorney General John Kroger said in a statement. "Given the lethal consequences of delaying detection of such a deadly cancer, I am giving medical impostors fair notice that these types of misrepresentations will not be tolerated."
Thermography in the spotlight
The Oregon case raises intriguing questions about infrared thermal breast imaging, which has been offered as an alternative or adjunct to mammography for years, but has never caught on in mainstream clinical practice.
Thermography is based on the principle that chemical and blood vessel activity in precancerous tissue is higher than in healthy tissue; thermal imaging cameras detect and analyze these temperature and vascular changes. Much of the technology's claim to validity stems from a U.S. Food and Drug Administration (FDA) approval of infrared thermal imaging as an adjunct breast cancer screening tool in 1982, according to Flir Systems of Boston, a maker of infrared thermal imaging cameras that have been used in thermography devices.
One of the technology's key weaknesses is that it has never been proved clinically, according to Dr. Leonard Berlin, chair of radiology at Rush North Shore Medical Center in Skokie, IL.
"There are no trustworthy clinical data out there that show thermography has any value at all," Berlin said.
It doesn't help that breast thermography has gotten a bad rap from users who have claimed just what the Crandalls did -- that it can replace mammography, according to Robert Kane, chiropractor and founder of Kane Infrared Interpretation Services in Redwood City, CA. Kane reads thermography images for more than 25 centers across the U.S.
"For a long time, thermography advocates touted it as a replacement for mammography," Kane said. "But it's not intended to do that. Thermography offers a different type of information, not for screening, but for breast cancer risk assessment. It's the step before mammography screening. Modern thermography is not about competing with radiology."
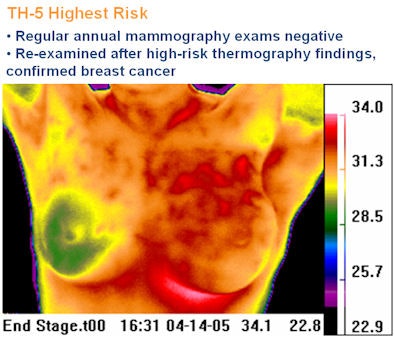 |
| Image courtesy of the Thermography Clinic, Toronto, Canada. |
In addition to a lack of clinical evidence, the technology is hindered -- and vulnerable to abuse -- because it is not covered by insurance carriers. Women who are already anxious about their breast cancer risk are more inclined to pay for the test out of pocket.
Thermography may be an interesting concept, but it has not proved practically useful, according to Dr. Daniel Kopans, professor of radiology at Harvard Medical School and senior radiologist in the Breast Imaging Division at Massachusetts General Hospital, both in Boston.
"Thermography is the same technique that is used to evaluate homes for heat losses from faulty insulation," he said. "If your house is well insulated, then a thermographic image will not detect a roaring fire in the fireplace. Breast tissue is a good insulator. It's likely that if a cancer produces heat, it will not reach the skin and will not be detectable by measuring the skin temperature. So thermography may be a nice idea but, thus far, has not worked for breast cancer detection."
By Kate Madden Yee
AuntMinnie.com staff writer
May 25, 2009
Related Reading
Thermal imaging measures inflammatory arthritis activity, February 23, 2006
Frost predicts tripling of non-mammo breast imaging in U.S., December 9, 2003
FDA approves small thermography camera, March 14, 2003
Thermal imaging market for breast cancer heats up, January 27, 2000
Copyright © 2009 AuntMinnie.com