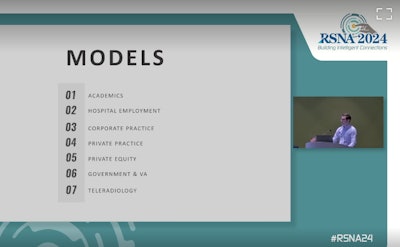
Navigating early career options presents more choices for radiology trainees than in the past. A special session at RSNA 2024 helped them prepare for decisions ahead.
Private equity ownership has been much talked about over the past few years for its role in changing the private practice landscape. However, private equity ownership accounts for only about 10% of the radiology market year over year, explained Eric Rubin, MD, who led the panel discussion. A diagnostic radiologist who recently joined Ochsner Health in New Orleans, LA, after partnering at Southeast Radiology in Pennsylvania, Rubin expects consolidation in radiology to continue.
"Maybe consolidation is good," Rubin told residents. "Maybe it allows better opportunities for work life balance because someone else takes care of the business if that’s what you want, but I do wonder if it’s the right thing to do for the profession. We are in a phase where radiologists are willingly giving away independence and, seemingly, losing interest in opportunities to build something for themselves in the future. We are just learning about the tradeoffs as they evolve in real-time."
"Private discussions that I’ve had suggest that the choice of private equity ownership by many is often a matter of survival in this environment and not necessarily to enrich senior partners," Rubin said. "We’re seeing economies of scale that are needed as volumes are exploding, as reimbursements are continuously eroding, regulatory burdens continue to make it more difficult to deal with the noninterpretive work that we do, and overhead costs are increasing at the same time."
Citing the American College of Radiology's 2023 Workforce Survey, Rubin highlighted private practice erosion and a significant 42% drop from dominance among radiology practice types. Further, Rubin said the survey showed a trend back toward academia.
To residents, Rubin recommended introspection: "about what you want from your career and how that interacts with your work-life balance."
Key points from the session, which was moderated by Brandon Fields, MD, a radiology resident at the University of California, San Francisco, and included a Q&A session with "private practice evangelist Ben White, MD, of American Radiology Associates in Dallas, Texas; Aaron Schein, MD, of Rolling Oaks Radiology in Thousand Oaks, CA; Olga Pasternic Wise, MD, from University of Chicago Medicine, Suhny Abbara, MD, from UT Southwestern Medical Center in Dallas, and Rubin:
- Most radiologists are staying put, but certain cohorts are more likely to seek new employment. They include those who work overnight, those who feel that life is balanced more toward work than life, and radiologists seeking to reduce their work hours during their first five years in practice. These environments could lead to more private practice erosion.
- A small but growing proportion of retired radiologists may be interested in getting back into the workforce, as seen in 2023 at 12% compared with 3% in 2021. Most of those interested were working part-time before they sought retirement. Depending on the data source used, the radiology specialty may see a net decrease in the number of radiologists in the U.S. by 2030.
"It’s really hard to pin down the number of radiologists in this country," said Rubin, who has served as chair of the ACR Commission on Human Resources. "Nobody can answer the question. We’re gonna get that data right at some point."
Rubin added, "You hear a lot of talk about how we need to increase the number of trainees to help our workforce shortage. That is not a short-term solution. We need to concentrate on other things to help us with short-term mitigation." - Advanced imaging volumes are projected to rise up to 20% by 2033. Without enough radiologists to handle increases, new solutions will need to evolve to manage the volume and evolve from within the specialty preferably, said Rubin, recalling when PACS and digital dictation provided relief years ago. On another note, nonphysician practitioners order at a higher rate, as AuntMinnie has already reported. The compound effect of this will become a problem in search of a disruptive solution, Rubin said during the talk.
"The solution isn’t to restrict access to valuable advanced imaging such as [for example, CT angiography] CTA, but to provide referring physicians with a frictionless way to evaluate the appropriateness of imaging," Elizabeth Rula, PhD, executive director of the Harvey L. Neiman Health Policy Institute explained in a July ACR blog. - Market disruptors, such as relaxing scope of practice guardrails on nonphysician practitioners, AI regulatory change, and allowing and reimbursing overseas imaging interpretation could pose a threat to radiologists' salaries, which historically have been the highest paid among medical specialists, according to Rubin. Radiologists should be involved in decisions about the future of radiology and radiologists, but Rubin also noted that it may become harder to motivate radiologist activists, especially when many will be employed rather than practice owners.
- AI, especially noninterpretive AI, will become significant in radiology practices. Simply saying no will likely exclude radiologists from the conversation.
- Compensation between private practice and academia is narrowing. Over time, academic radiologists have been reading more [relative value units] RVUs and getting paid better. The corporatization model has taken over, no matter where you work, White discussed. Pasternak Wise added that academic centers are moving into a hybrid model to improve recruitment. Also, tenure track has become something to shy away from, except for PhD scientist tenure track, according to Abbara.
- Dollar per dollar, RVU is context-dependent. A job that is almost all remote with flexible hours is a very different job than working for a hospital.
"You cannot evaluate a single job based on a big trend," said White, a self-described private practice evangelist and neuroradiologist and partner at American Radiology Associates. White also serves as associate program director at the Baylor University Medical Center Radiology Residency. Don't discount the benefits of community and variety that comes with academia, he said. - The field of radiology is malleable. No matter what you are doing at the moment, there is more than one way out, said Schein, whose career choices allowed him to prioritize starting a family. "You can adapt to personal circumstances ... different areas of specialization," he said.
- Partnerships today mostly involve buying into the professional component, rather than the technical component or both. Ownership opportunities of equipment and centers are decreasing over time, in part because of ongoing erosion of technical component reimbursements, especially on the outpatient side.
"I think that the concept of what partnership means may not be as important as it has been historically," Rubin said. At the same time, White encouraged residents to increase their value to their organization, with "boots on the ground" contributions and being part of the culture. "At what sticker price value is partnership? It’s not zero to me," he said. - Teleradiologists are not what most radiology practices really need right now. Everyone can't have a teleradiology job without destabilizing the entire industry, White said.
This session, "Navigating the Job Market," was sponsored by the RSNA Resident and Fellow Committee.