Renal Collecting System Obstruction
Although some use the terms hydronephrosis and hydroureter to describe dilatation of the collecting system secondary to obstruction, and the terms caliectasis and pelviectasis denote dilatation, but not necessarily obstruction, others use the term hydronephrosis to describe non-specific collecting system dilation. Causes of hydronephrosis and hydroureteronephrosis include
- Obstruction
- Previous obstruction
- Vesicoureteral Reflux
- Recent urinary tract infection
- Congenital malformations
- Noncompliant bladder
When the obstruction is complete, the renal parenchyma atrophies completely and renal size decreases. In partial obstruction, the degree of parenchymal thinning is directly proportional to the severity of obstruction. Glomerular function (evaluated with Tc-DTPA) is more sensitive to ureteral obstruction than is tubular secretion (evaluated with MAG3), although once tubular changes occur, they take longer to reverse.
The Whitaker test (pressure perfusion study) has been considered the gold standard for distinguishing obstructive from non-obstructive hydronephrosis. However, this status has been questioned because of non-physiologic flow rates, lack of pediatric normal limits, presence of an indeterminate range in a purported gold standard, and lack of studies corelating its results with deterirating function. The exam measures the pressure within the renal pelvis under conditions of increased flow. A pressure greater than 22 cm H2O at a flow rate of 10 mL/min. is felt to be representative of obstruction (normal is less than 15 cm H2O). Unfortunately, the examination is invasive (a percutaneous nephrostomy is required) and fails to provide any information regarding renal function. At the present, many believe that a prospective imaging gold standard does not exist for chronic obstruction, and that the diagnosis is made retrospectively by demonstrating loss of function or relief of symptoms with an intervention. Assymptomatic hydronephrosis without obstruction is not associated with increased morbidity.
Although there is general agreement that diuretic renography is accurate in adults, recent opinion is changing in neonates and infants. The recent trend in infants is toward less agressive operative management of the dilated asymptomatic collecting system, even when unilateral poor function or obstructive diuretic renography findings are present on initial scanning [1], since the natural history of dilation seems to be resolution or stability of dilation and renal function in this group.
Furosemide Renography
Technique
The examination can be performed on neonates less than one month old [4]. Prior to the exam oral hydration should be offered as libitum, as formula or water beginning 2 hours before the study and throughout the exam [4]. IV fluid should be given as a dilute saline solution (D5 0.3 NS or D5 0.25 NS) at a rate to deliver 15 mL/kg over a 30 minute interval, beginning 15 minutes before injecting the radiopharmaceutical [4]. The infusion is continued for the remainder of the study ay a maintenance fluid volume at a rate of 200 cc/kg/24 hours [4]. The patients bladder should be catheterized to ensure adequate drainage throughout the study, although this practice is not universal [4]. Most children do not have neurogenic bladders or bladder outlet obstruction and will void spontaneously [4]. Catheterization may be required for children with grade II vesicoureteral reflux or higher [4]. A wide clinical variance in the performance furosemide renography has led to the publication of three consensus statements which are very similar in their methods and interpretive criteria:
- SNM Nuclear Medicine Procedure Guidelines for Pediatric Diuretic Renography
- The "Well Tempered Diureitic Renogram" [2]
- Consensus statement from the 9th International Radionuclides in Nephrourology Meeting, Committee on Diuretic Renography [3]. This statement had the most detailed recommendations for interpretation.
Areas of disagreement in these statements are the need for IV hydration and indwelling catheter in all patients, and type of IV fluid used and flow rates.
Tc-MAG3 is the agent used for the examination at a dose of 1.85 MBq/kg (50uCi/kg) and a minimum doseage of 37MBq (1mCi). The patient is supine during the exam. Digital data (at 20 sec/frame) and analog images are acquired [4]. Lasix is injected IV at a dose of 1mg/kg at 20-30 minutes after tracer administration or when the enire collecting system is believed to be full [4].
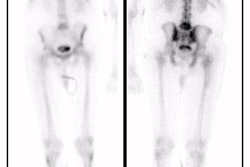
Nondiuretic renography is extremely sensitive but very non-specific for obstruction. Furosemide renography is based on the principle that prolonged retention of tracer in a dilated, non-obstructed collecting system is due to a reservoir effect and that diuresis will cause increased urine flow through the collecting system which should "wash out" the activity. In the presence of significant obstruction, the urinary tract is unable to clear and activity will not change significantly.
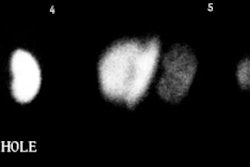
A collecting system without significant obstruction will have a clearance half-time (ie: the time for half of the activity present to clear) following the administration of furosemide of less than 10 minutes. Greater than 20 minutes is abnormal and is associated with high grade obstruction. Clearance half-times between 10 and 20 minutes are considered indeterminate, but the patient should be followed closely. The T1/2 is best measured from the point of response to furosemide (not necessarily from the point at which furosemide is given). The response to furosemide usually begins 1 to 2 minutes after injection, and maximum diuresis may not be reached until 15 minutes in some patients.
The T1/2 should not be the sole criterion upon which a determination of obstruction is based. Its value should be interpreted in conjunction with the other data available from the exam- curve analysis, differential function, and visual analysis of the acquired images. The washout curve from a nonobstructed kidney is more likely to have an exponential or concave shape, even if washout is prolonged. A convex shape is more indicative of obstruction. A biphasic curve (one which drops quickly, but then levels off at a high level or even rises) is almost always indicative of a flow dependent obstruction- particularly when the curve levels off above 30% of retained activity.
Improvement in the washout of the tracer after pyeloplasty varies greatly. In many cases, the half-time remains in the obstructed or equivocal range for at least 6 months. If function remains stable during this interval, however, there is no need for concern.
Factors which affect half-time clearance include:
1- Urine flow rate response to the diuretic:
- Patient hydration status: Dehydrated patients will have less of a response. Therefore, adequate hydration is essential for diuresis. Adults should consume 300-500 ml of water prior to the exam. In infants and children, 5% dextrose in one-third normal saline (15 ml/kg) is infused over 30 minutes prior to the exam (WTDR)
- Diuretic dose: 1mg/kg up to 40 mg has been shown to be optimal. In very obese patients or in patients with impaired renal function, doses larger than 40 have been proposed, although the Radionuclides in Nephrology consensus statement points out that there is no data to support increased furosemide doses in azotemic patients. Maximum diuresis usually occurs within a few minutes after furosemide injection in the hydrated patient.
- Degree of renal insufficiency: The urine flow rate following furosemide is roughly
proportional to the creatinine clearance. Adequate diuresis is possible even at creatinine
clearances as low as 10ml/min. In general, when the collecting system does not completely
fill within one hour after injection (ie: persistent parenchymal activity) or when the
affected kidney has less than 20% of the total renal function, a prolonged washout is not
be a reliable indicator of obstruction. [Nuclear Medicine in Pediatric Urology, Majd,
p.129] The Radionuclides on Nephrology consensus statement recommends that a single kidney
GFR (SKGFR) be used in interpreting the significance of abnormal T1/2 and renogram curve
shapes:
- The negative predictive value for a normal T1/2 and curve shape is high in all cases.
- SKGFR > 15ml/min with an obstructive curve should be interpreted as obstructed.
- SKGFR < 15ml/min with obstructive or indeterminate curve should be interpreted as indeterminate, not partially obstructed.
- SKGFR > 15ml/min with an indeterminate curve should be interpreted as probably obstructed.
2- Volume of the dilated collecting system
Massive hydronephrosis can result in apparently abnormally prolonged clearance.
T1/2 is directly proportional to the collecting system volume.
T1/2 = k (Collecting system volume)/flow rate
3- Distortion of true activity in the collecting system
Background activity or prolonged cortical retention of tracer can both affect the calculated clearance time.
4- Functional Obstruction
a. Distended Bladder
A distended bladder may prolong clearance due to the increased intravesicular pressure which will slow collecting system drainage or the presence of vesicoureteral reflux. An indwelling foley catheter will eliminate this effect, as well as permit measurement of urine output and decrease the radiation dose to the gonads.
b. Postural stasis
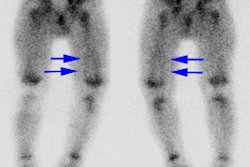
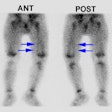
Certain patients may drain completely when erect. It is essential that a standing/upright post-void viewbe obtained. In children, prone imaging should be performed if there is delayed clearance on supine images. Markedly improved drainage in the prone position makes high grade obstruction unlikely, and is usually associated with preservation of renal function.
(1) J Urol 1994;152: 593-5
(2) Semin Nucl Med 1992; Conway JJ. "Well-tempered" diuresis renography: its historical development, physiological and technical pitfalls, and standardized technique protocol. 22: 74-84
(3) J Nucl Med 1996; O'Reilly P, et al. Consensus on diuresis renography for investigating the dilated upper urinary tract. Radionuclides in Nephrourology Group. Consensus Committee on Diuresis Renography. 37(11):1872-6
(4) J Nucl Med 2001; Rossleigh MA. Renal cortical scintigraphy and diuresis renography in infants and children. 42: 91-95