Congenital Diaphragmatic Hernia:
Clinical:
Congenital diaphragmatic hernia occurs in approximately 1 in 2,200-2,500 live births [3,5]. The lesion is unilateral in 97% of cases [4]. The lesion occurs most commonly on the left, posteriorly through the foramen of Bochdalek (90%). If the viscera dislocate during early lung development the ipsilateral lung will hypoplastic and contralateral hypoplasia may also be seen due to compressive effects of the herniated abdominal contents [4]. Symptoms include respiratory distress at birth, however, if the defect is small, patients may not be symptomatic and they may go undetected. The hernia may be delayed on the right. Associated anomalies are found in 25% of cases and include GI malrotation, omphalocele, left heart hypoplasia, pulmonary sequestration, and neural tube defects (28%). Intrauterine growth retardation is found in nearly 90% of cases. About one third of affected children are still born, and another third die in the neonatal period. The mortality is influenced by the degree pf lung hypoplasia and the presence of persistent pulmonary hypertension [5].Treatment consists of immediate surgical repair, assisted mechanical ventilation, and possibly extra-corporeal mechanical oxygenation. Survival rates are between 41-75% and survival is related to the degree of pulmonary hypoplasia. Predictors of improved survival are diagnosis after 25 weeks gestation, smaller degree of pulmonary hypoplasia, and the lack of liver in the chest. [1,2]
Antenatal therapy can be offered in a select group of fetuses predicted to have lethal pulmonary hypoplasia in whom the chances for survival are low (<15%) [5]. Antenatal intervention is performed to trigger lung growth rather than correct the diaphragmatic defect, which can be easily repaired after birth [5]. Temporary tracheal occlusion is performed to prevent egress of lung fluid produced by the airway epithelium and induces tissue stretch which acts as a signal for lung growth [5]. Subsequent prenatal release of the occlusion stimulates lung maturation [5]. Percutaneous fetoscopic endoluminal tracheal occlusion is performed using a balloon device [5]. The survival rate is approximately 50% [5].
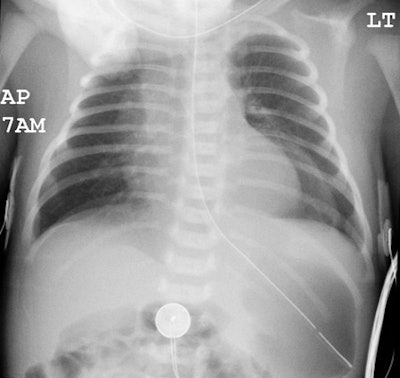
X-ray:
Prenatal sonography is able to detect the presence of bowel within the chest, however, the diagnosis may be missed in up to 41% of cases. Magnetic resonance imaging may be more sensitive to the detection of liver within the chest than sonography. (1)On prenatal MR, fetuses with a relative lung volume of less than 14% typically die, while those with a volume greater than 33% survive, and those with a volume greater than 44% generally do not require extracorporeal membrane oxygenation [4].
On plain film there is a scaphoid airless abdomen and there are generally multiple air and fluid filled loops of bowel within the thorax, however, if very early, the hernia may appear as a solid density (infant has not yet swallowed enough air to fill the hernia). The heart and mediastinum are displaced to opposite side of the hernia and there is compensatory hyperinflation of the opposite lung. The lesion may be identified on prenatal ultrasound and is characterized by polyhydramnios due to a functional obstruction at the EG junction, mediastinal shift secondary to mass effect, and abnormal upper abdominal anatomy.
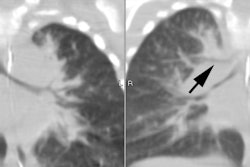
Unsuspected congenital diaphragmatic hernia: The newborn shown below presented with respiratory difficulty, but did not have a scaphoid abdomen. The frontal CXR demonstrated and abnormal lucency and curvilinear density in the left base. A lateral view revealed findings concerning for a diaphragmatic hernia. This was confirmed on CT imaging- note that a portion of the stomach and the spleen have herniated through the defect. |
|
REFERENCES:
(1) Radiology 1997; 203: 636-640
(2) AJR 1999; Donnelly LF, et al. Correlation between findings on chest radiography and survival in neonates with congenital diaphragmatic hernia. 173: 1589-1593
(3) AJR 2008; Ruano R, et al. Predicting neonatal deaths and pulmonary hypoplasia in isolated congenital diaphragmatic hernia using sonographic fetal lung volume-body weight ratio. 190: 1216-1219
(4) Radiographics 2010; Daltro P, et al. Congenital chest malformations: a multimodality approach with emphasis on fetal MR imaging. 30: 385-395
(5) Radiology 2010; Breysem L, et al. Cross-sectional study of tracheomegaly in children after fetal tracheal occlusion for severe congenital diaphragmatic hernia. 257: 226-232