Pairing 5-fluourouacil (5-FU) chemotherapy with preoperative radiation can increase tumor response to treatment and potentially contribute to sphincter preservation in rectal cancer patients, according to a new study.
Researchers at the M.D. Anderson Cancer Center in Houston and Washington University in St. Louis teamed up to compare outcomes from preoperative chemoradiation and radiation therapy in patients with stages T3 and T4 low rectal cancer.
"Improved local control and survival is achieved with preoperative radiation therapy than with surgery alone...over the past 10 years, preoperative chemoradiation has been used at (M.D. Anderson) ...at Washington University, the routine policy through 1995 was to give preoperative radiation therapy alone...however, there has been an increasing use of concurrent chemotherapy," wrote Dr. Christopher Crane and colleagues in the International Journal of Radiation Oncology, Biology, and Physics (September 1, 2003, Vol. 57:1, pp. 84-89).
The study focused on 403 patients from both institutions with clinically staged T3 and T4 adenocarcinoma of the rectum. In all cases, the lower border of the tumor was less than or equal to 12 cm from the anal verge. Of the 403 patients, 215 were treated with concurrent chemotherapy and radiotherapy, while 188 underwent radiation therapy alone. The work-up for staging included abdominal and pelvic CT, chest x-rays, blood tests, and colonoscopy.
The preoperative radiotherapy technique generally consisted of 18 MV high-energy photons delivered to the posterior pelvis. All patients at M.D. Anderson received 45 Gy in 25 fractions over five weeks. At Washington University, 26 patients received 20 Gy in five fractions of 5 Gy, followed by surgery within 1-2 days. Senior attending surgical oncologists, specializing in colorectal cancer, performed the operations, including resection of the primary tumor with margins of normal tissue around the tumor site.
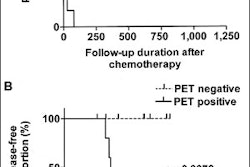
Kaplan-Meier methodology was used to estimate the actuarial pelvic disease control rates (PC), relapse-free survival rates (RFS), and overall survival rates (OS).
According to the histologic results, patients treated with preoperative radiation alone had a complete response rate of 5%. M.D. Anderson patients treated with preoperative chemoradiation had a complete response rate of 23%; those at Washington University had a 13% complete response rate. In terms of downstaging, patients treated with preoperative chemoradiation at Washington University (after 1995) showed a downstaging rate of 42%.
"Patients with low rectal tumors (less than or equal to 6 cm from the anal verge) underwent sphincter-preserving procedures more commonly than those with an incomplete histologic response (43% vs. 27%)," the authors stated.
Overall, the use of concurrent chemotherapy with preoperative radiation improved tumor response and pathologic complete response, but did not significantly improve PC, RFS, or OC.
The results of an ongoing randomized trial being conducted by the European Organization for Research and Treatment of Cancer (EORTC) should offer further evidence of concurrent chemotherapy with radiation in a preoperative setting, the authors noted.
By Shalmali PalAuntMinnie.com staff writer
September 25, 2003
Related Reading
New treatment approach improves local control of rectal cancer, June 20, 2003
No size, grade correlation seen in enhancement of colorectal cancer, June 9, 2003
Copyright © 2003 AuntMinnie.com