The most commonly used drug class in the world, nonsteroidal anti-inflammatory drugs (NSAIDs), are associated with a host of proven benefits, primarily their ability to control pain and inflammation due to acute or chronic conditions. Drugs in this class are also being investigated for several potential preventive benefits, including colorectal cancer, Alzheimer’s disease, and, most recently, Parkinson’s disease.
Unfortunately, the information on NSAIDs’ adverse effects keeps accumulating, too. Some researchers have reported a link between long-term NSAID usage and musculoskeletal defects. Others are reporting an increased chance of miscarriage in women who regularly take NSAIDs. Most recently, investigators from Israel reported that low-dose aspirin therapy might have a "significant adverse effect on renal function" in elderly patients (American Journal of Medicine, October 15, 2003).
Others are going even a step farther to prevent certain patients from ever swallowing their first NSAIDs pill. A group at Kaiser Permanente Southern California in Downey has developed an assessment model to predict whether certain patients run the risk of gastrointestinal (GI) bleeding when treated with NSAIDs. The study followed over 300,000 NSAID users, 302 of whom were hospitalized for a GI bleed. The authors found a link between NSAIDS, patient age, and a history of GI bleed (Journal of Rheumatology, October 2003, Vol. 30:10, pp. 2241-2244).
The medical community is growing more aware that, as prevalent as NSAIDs are, they may not be for everyone. Enter imaging, specifically CT and MRI, to document the potential damage caused by long-term NSAID use.
Treating a broad class of illnesses
People take a host of over-the-counter NSAIDs for back pain, other transient joint pain, and as an ongoing treatment for osteoarthritis. The common players are aspirin, ibuprofen, and naproxen. Ibuprofen is often also used to control fever and to control pain after dental surgery. Low-dose aspirin is often taken long-term for its platelet aggregation properties to prevent secondary myocardial infarction.
Certain NSAIDS, such as diclofenac (Voltaren) and the newer, more selective NSAIDs, or cyclo-oxygenase 2 (COX-2) inhibitors, such as rofecoxib (Vioxx) and celecoxib (Celebrex), are only available by prescription and are typically prescribed to manage joint pain related to either osteoarthritis or rheumatoid arthritis. Methotrexate, technically a disease-modifying anti-rheumatic drug (DMARD), is also anti-inflammatory and is used to treat autoimmune conditions such as rheumatoid arthritis and psoriasis, and has recently been investigated for asthma.
Several studies this year added to the body of literature showing NSAID-related injury to both the musculoskeletal system as well as to various organs. Dr. David Nag presented information at the 2003 American Roentgen Ray Society conference in San Diego showing that NSAIDs are linked to "severe destructive arthropathy with irregularity of both femoral head and acetabular surfaces" as confirmed on MRI.
Over an 18-month period, Nag and his colleagues had 14 patients who initially presented with hip pain. Out of the 14, 11 were known to be on NSAIDs. All of the patients underwent radiography while six had MR scans. The MRI showed "marked bone destruction of (femoral head and acetabular surfaces) with reactive marrow edema and a fluid component," (American Roentgen Ray Society abstract book, May 2003, Vol.180:3, p.5).
Nag, a clinical radiologist at the Hull Royal Infirmary in Hull, East Yorkshire, U.K., stressed that an MRI could only confirm the damage, although an MRI was "not conclusive" that the joint erosion could be attributed to NSAID use.
Others have made a more direction connection between NSAIDs and negative side effects. Dr. De-Kun Li and co-authors published a study showing a link between NSAID use and miscarriage. Li, an epidemiologist with the Kaiser Foundation Research Institute in Oakland, CA, wrote that in a study of 1,055 pregnant women, 53 (5%) were using NSAIDs around the time that they conceived or during their pregnancies. Those women were 80% more likely to miscarry than were the other women, and the risk increased if the treatment lasted for a week or longer.
Li attributed this link to the prostaglandin-inhibiting effect associated with this drug class, and noted the critical role of prostaglandins for implantation (British Medical Journal, August 16, 2003, Vol. 327:7411, p. 368).
These recent findings reinforce prior research showing that long-term NSAID use can bring an unwanted package of complications. The injuries most commonly associated with NSAIDs typically affect the gastrointestinal tract.
 |
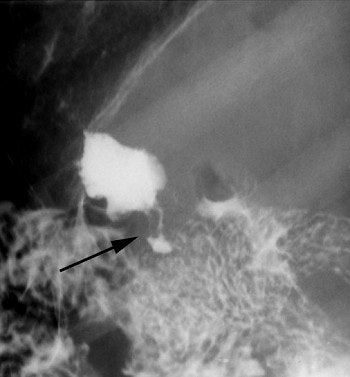
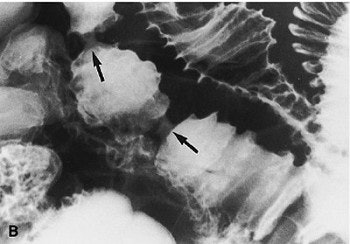
Above, an example of a pyloric channel ulcer (black arrow). Below, a spot compression view. Ulcers are often associated with NSAID usage.
 |
Dr. Sung Eun Rha of the Catholic University of Korea in Inchon, South Korea, documented a case of a duodenal diaphragm associated with long-term NSAID use in a 55-year-old man who had been treated with both NSAIDs and steroids for four years to relieve hip pain due to avascular necrosis (American Journal of Roentgenology, September 2000, Vol. 175:3, pp. 920-921).
Rha pointed out that other researchers had suggested that duodenal diaphragm may be a consequence of small intestine circumferential ulceration. Similarly, Dr. Arthur Zalev, professor of radiology at the University of Toronto, documented cases of NSAID-related small intestine injury.
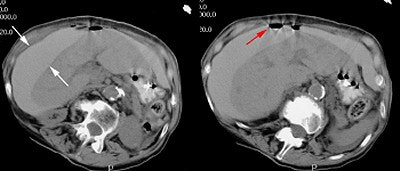 |
| CT scan from a patient with a perforated gastric ulcer. The patient presented with severe abdominal pain. Oral contrast given prior to the exam can be seen free within the peritoneal cavity about the liver (white arrows). There is also free air (red arrow). The findings are consistent with a perforated viscus. |
Additionally, other investigators had reported thoracic injuries. Dr. Masanori Akira, chief of radiology at the National Kinki Chuo Hospital for Chest Disease in Sakai City, Osaka, Japan, identified cases of drug-induced pneumonitis on thin-section CT scans (Radiology, September 2002, Vol. 224:3, pp. 852-860).
Drs. Samantha Ellis and Nestor Müller also identified aspirin in particular as a cause of salicylate-induced acute respiratory distress syndrome, and noted that methotrexate can also cause pulmonary toxicity. Ellis and Müller pointed out that high-resolution CT can identify signs such as interstitial pneumonitis, centrilobular nodules, or localized nodular air-space filling patterns (AJR, October 2000, Vol. 175:4, pp. 1019-1024).
Appropriate imaging modalities
Not surprisingly, the appropriate imaging modality to document NSAID-related injury depends on the anatomic part involved. For musculoskeletal involvement, MRI provides more definitive images than CT, x-ray, or ultrasound, according to Nag.
For gastrointestinal injuries, the key findings range from a narrowing of the pyloric canal with distension of the duodenum’s first and second portions, fistulae, strictures, and erosions in the esophageal lining. A variety of modalities can document such signs. Rha’s team used delayed-compression spot radiography to document duodenal diaphragm, and confirmed it with exploratory laparoscopy.
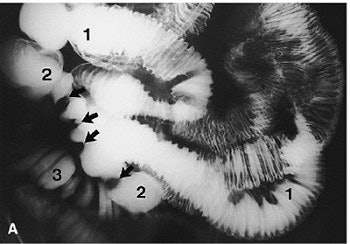  |
Overhead view (A) shows three abnormal jejunal loops. Four broad-based strictures with lumps are seen in loop 2 (arrows). Compression spot view of loops 1-2 (B). Marked luminal narrowing in two of the four strictures in loop 2 (arrows) is seen with a resultant life-saver or bagel-like configuration. Compression spot view of loop 3 (C). Multiple ring or diaphragm-like strictures (arrows) and broader-based strictures (arrowheads) are evident. Images courtesy of the Canadian Association of Radiologists (Abdominal Imaging, 1998; 23:40-44).
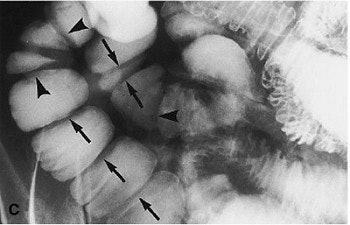 |
Similarly, Zalev and his co-investigators coupled CT with laparotomy. In one of Zalev’s case studies, a 60-year-old woman presented with multiple symptoms, including malabsorption. She had used NSAIDs for many years after bilateral total hip replacements. "A small-bowel CT scan showed a long jejunal segment with mucosal edema and multiple strictures," the authors wrote (Abdominal Imaging, January-February 1998, Vol. 23:1, pp. 40-44).
 |
| CT scan with oral and intravenous contrast through the plane of loop 3 (arrows) showing the strictures. Zalev, AH, Gardiner GW, Warren RE, "NSAID injury to the small intestine" (Abdominal Imaging, 1998; 23:40-44). |
Dr. Perry Pickhardt, a staff radiologist at the National Naval Medical Center in Bethesda, MD, identified gastrointestinal fistulae due to several etiologies, and noted that cross-sectional imaging, either with CT or MRI, can be useful, and that fluoroscopy can complement these two.
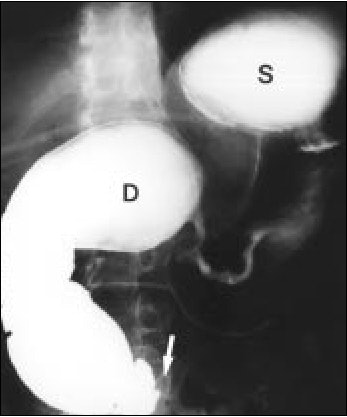 |
| Upper gastrointestinal radiograph shows smooth narrowing of pyloric canal and marked distension of first and second portion of duodenum (D). Also, note marked passage disturbance at third portion of duodenum to distal bowel loops (arrow). S is the stomach. Rha, SE, Lee JH, Lee SY, Park, SM, "Duodenal diaphragm associated with long-term use of nonsteroidal anti-inflammatory drugs: a rare cause of duodenal obstruction in an adult," (AJR 2000, Vol. 175, pp. 920-921). |
In their review in Radiology, Pickhardt and colleagues laid out the role of imaging in the detection of acquired gastrointestinal fistula. Their classification scheme included separating the fistulas into either acquired or congential, external or cutaneous.
"The preferred imaging approach will vary according to fistula type and the specific clinical scenario," they wrote. Some of imaging techniques they recommend were contrast-enhanced fluoroscopy, fistulography, small bowel studies, and enteric contrast-enhanced studies.
"Although CT may be less sensitive for direct detection of some GI fistulas...CT often yields more valuable information overall with respect to patient care," they said. "Often, CT directly or indirectly demonstrates the presence of GI fistula, elucidates the underlying cause, and obviates further imaging (Radiology, July 2002, Vol. 224:1, pp. 9-23).
The same holds true for CT and thoracic injuries, according to Dr. Masanori Akira and colleagues in their Radiology paper. On high-resolution CT, the most common findings of NSAID-related lung disease may be areas of ground-glass opacity with interstitial thickening and centrilobular opacities, Akira told AuntMinnie.com, "noting that these areas reflect the allergic reaction. Some patients may show peripheral consolidation and drug-induced eosinophilic pneumonia, while others may have non-cardiogenic pulmonary edema. The best imaging modality for identifying NSAIDs-related lung disease is high-resolution CT."
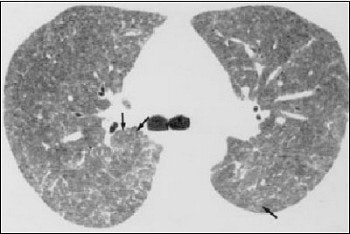 |
| Fifty-two-year-old man with hypersensitivity reaction; patient was receiving methotrexate for rheumatoid arthritis. High-resolution CT scan shows poorly defined centrilobular nodules (arrows) and extensive areas of ground-glass attenuation. Differential diagnosis includes interstitial pneumonitis related to rheumatoid arthritis, opportunistic infection, and adverse drug reaction. Diagnosis was confirmed at open lung biopsy. Ellis SJ, Cleverley JR, Müller NL, "Drug-induced lung disease: high-resolution CT findings (AJR 2000, Vol.175, pp.1022-1027). |
Regardless of the imaging modality used, Akira cautioned that when it comes to tracking NSAIDS injuries, no two are alike.
"The imaging findings of drug-induced lung disease vary among patients and drugs," he warned. "The same drug may produce more than one pattern."
By Paula MoyerAuntMinnie.com contributing writer
November 27, 2003
Related Reading
Tiny camera shows fewer bowel lesions with Celebrex, October 16, 2003
Given Imaging to debut M2A Patency System, October 7, 2003
Painkillers may raise lymphoma risk for women, September 15, 2003
'Fantastic voyage' into gut nearer to reality, May 21, 2003
Molecular imaging explains why ibuprofen prevents Alzheimer’s, April 8, 2003
Copyright © 2003 AuntMinnie.com