Developed more than 30 years ago, computer-aided detection (CAD) technology has continued to evolve as computers have become more powerful. Although clinical applications of the technology have traditionally been limited to mammography, companies are rapidly developing techniques for use with other modalities.
CAD aims to offer a "double read" that requires fewer resources than a second radiologist, with some important successes. Researchers have shown, for example, that CAD can help doctors find almost 20% more breast cancers than they would have without using the technology. According to R2 Technology (Sunnyvale, CA), more than six million screening mammograms in the U.S. will be interpreted with CAD assistance this year, or about 15% of all screening mammograms in the U.S.
And CAD is moving out of the sole province of 2-D modalities like mammography or chest, and into 3-D applications using CT and MR. The technology is being applied to multiple image data sets with hundreds or thousands of images, wherever the problem of observational oversight and productivity for the radiologist is an issue, according to Susan Wood, Ph.D., vice president of R2’s CT products division.
"With a modality like multislice CT, the end user is creating a moratorium on technology advances because the data output is unmanageable," Wood said. "CAD could be part of managing higher-resolution data that is acquired at faster speeds."
CAD developers also have high hopes that the technology will move into the realm of computer-aided diagnosis as it gets increasingly sophisticated in its sensitivity and specificity. This might be useful in situations where a community can’t afford a radiologist, though the issue is controversial. Other potential uses for CAD include helping physicians detect diseases like tuberculosis or SARS and combining CAD with dual-energy DR or CR to improve the detection of chest disease.
Consensus in clinical community
Most would agree that CAD for mammography is well accepted, even if not every facility can afford a CAD unit. As the technology begins to migrate to other modalities such as CT and MRI, which produce large quantities of data, the expectation among CAD developers is that doctors’ receptivity to CAD will remain high.
It helps that Medicare reimburses for CAD. The current reimbursement level is $19.13 ($15.82 for the technical fee; $3.31 for professional). Medicare reimbursement for CAD began in 2001, with payment amounts increasing slightly a year later; also in 2002, the Center for Medicare and Medicaid Services (CMS) expanded CAD coverage to include diagnostic exams. This year the coverage was expanded to include the technology’s use with digital mammography.
More private payors are coming through as well, according to Peter Farrell, vice president of marketing for CADx Systems in Dayton, OH.
"There has been a groundswell of customers who want digital mammography and CAD, which has caused some private clinics to offer CAD as a service people can pay for themselves," Farrell said. But the question of cost-effectiveness remains for many facilities. Gerald Kolb, president of Breast Health Management of Bend, OR, estimates that the breakeven point is about 20 mammograms per day, or 5,000 per year; to make a profit, a center needs to perform 30 or more screening mammograms a day.
CAD does offer another edge: protection from liability. Radiologists are more often the targets of breast-cancer litigation than other specialists, and the average judgment is $300,000. Missed cancer or delayed diagnoses are common reasons for these suits.
CAD and breast imaging
There’s little doubt that CAD for mammography has had a significant impact on breast cancer screening. The ability to find small cancers earlier is the technology’s strength. In a 2001 study, Drs. Timothy Freer and Michael Ulissey screened 13,000 women over the course of a year, using conventional mammography reading techniques as well as CAD. They found almost 20% more cancers with CAD (Radiology, September 2001, Vol. 220:3, pp. 781-786).
But it is also clear that CAD will not soon replace an experienced radiologist. And CAD, it seems, does not always make for smoother logistics in the clinical setting: CAD can slow down workflow in a film-screen environment due to the time required to digitize each film.
When used with digital technology, however -- particularly modalities such as MRI -- the concern about throughput dissipates. An increasing number of outpatient imaging centers dedicated to women’s health issues are offering modalities such as MRI to image the breast, in addition to traditional modalities and methods of finding disease.
But despite clinicians’ interest in using MRI for breast cancer screening purposes, cost, training, and time/throughput concerns have slowed the adoption of MRI for this use, according to Dr. Justin Smith of First Hill Diagnostic Imaging of Seattle. CAD could help mitigate these factors, increasing patient throughput by automatically processing images according to a site’s or physician’s preferences. Other benefits are a potential increase in a radiologist’s efficiency by sifting through large datasets and highlighting suspicious areas; and addressing issues such as correcting artifacts caused by patient movement and standardizing image processing.
CAD and lung imaging
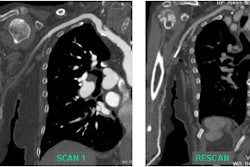
In a 2002 study published in American Journal of Roentgenology, researchers from Osaka University Graduate School of Medicine in Japan found that radiologists could better find hazy opacities on chest x-rays when they used a CAD unit that highlighted changes between current and previous radiographs (AJR, August 2002, Vol. 179:2, pp. 467-471).
The opacities were due not only to potential lung cancers, but also pneumonia and pneumonitis. These findings are part of what’s exciting about CAD and lung imaging, according to Mike Klein, president and CEO of R2 Technology. Until now, CAD has been used as a way to find cancers. But in applications such as lung imaging, it could be used to find other disease -- to mark anything that doesn’t "belong" in the image.
"What we’re finding in our lung cancer screening CAD is that we’re noticing things that remain on the image aren’t just cancer," Klein said. "We’re finding pulmonary embolism with CAD. The combination of a physician’s skill and CAD technology could lead to a much higher accuracy of detection of disease."
Although many radiologists are focusing on CAD with CT for lung cancer detection, using CAD with DR or CR technology could be a more practical means of initial cancer detection in terms of affordability, availability, and throughput, according to Michael Yeh, Ph.D., president and CEO of Rockville, MD-based Deus Technologies. CT alone, or CT with CAD, can then be used for follow-up, Yeh said.
CAD and virtual colonoscopy
CAD shows promise in this area, particularly because it could reduce the discomfort patients often feel during colonoscopy, as well as a small risk of perforation. CT-colonography, or virtual colonoscopy, performs 3-D volumetric reconstructions of the colon, producing huge datasets that have to be reviewed by doctors, often taking 20 to 30 minutes for each study. CAD could identify suspicious lesions and "fly through" the colon, identifying the particular areas of concern and reducing exam time. CAD developers hope that the technology will identify polyps that hide, and tout the technology’s ability to electronically remove tagged stool from the image -- a key factor in increasing patient compliance, according to Klein.
"Compliance for (conventional) colonoscopy is 15% (of the eligible population)," he said. "The prep is as bad as the test. CAD could change the protocol for how the procedure is done, which would make the prep easier and boost compliance."
A study published in RadioGraphics found that CAD technology has improved its ability to detect colorectal polyps with high accuracy and low false-positive rate. The group examined CT data for 71 patients (31 men and 40 women, age 32 to 84) who were referred for virtual colonoscopy. The CAD’s performance was measured by polyp and patient. By patient, CAD was 100% effective, with an average of two false-positive findings per patient. By polyp, CAD was 90% sensitive, detecting 19 of 21 polyps with the same false-positive rate (RadioGraphics, July-August 2002, Vol. 22:4, pp. 963-979).
Ongoing issues
What still needs work in CAD technology? Sensitivity and specificity. CAD developers continue to work on increasing their systems’ sensitivity while maintaining a reasonably low number of false-positives, each of which must be reviewed and eliminated individually. One lung CAD system even incorporated adjustable false-positive settings, offering radiologists a trade-off between high sensitivity and a high false-positive rate on one hand, and lower sensitivity with fewer false-positives on the other.
Another need is for more data to be added to the algorithms to improve CAD schemes’ ability to detect pathology even more precisely, according to CADx Systems’ Farrell. The more information from different sensors, patient history, HIS/RIS and prior image data that’s included, the more sensitive and specific CAD technology will be, he said.
In any case, CAD technology is in a refinement stage, and the clinical community will continue to see it being incorporated into more applications.
"Imagine a building, and all the rooms that were needed for the next ten years are already in place," Farrell said. "The foundation is already laid. Now we’re adding furniture."
By Kate Madden YeeAuntMinnie.com contributing writer
January 13, 2004
Related Reading
Virtual colonoscopy study results disappointing, August 13, 2003
Computer-aided detection enhances breast MRI, June 6, 2003
Effective breast CAD still harbors a few workflow caveats, June 3, 2003
CAD mass markers aid in reduction of mammographic interpretation errors, March 7, 2003
Why CT lung cancer screening will (and won't) work, November 11, 2002
CAD scheme offers faster, more accurate virtual colonoscopy, November 6, 2002
CAD highlights hazy opacities on chest x-rays, October 11, 2002
Copyright © 2004 AuntMinnie.com