Dear AuntMinnie Member,
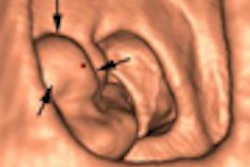
Advocates of coronary CT angiography (CCTA) are celebrating after the U.S. Centers for Medicare and Medicaid Services (CMS) yesterday announced that it was shelving a plan that could have radically restricted Medicare reimbursement for heart CT studies.
CMS said that it would not implement a proposal first broached in December to set a national coverage policy restricting CCTA payments to just two indications, according to an article we're featuring in our CT Digital Community. The policy would have overruled the current situation, in which local Medicare carriers are allowed to set their own reimbursement policies for the exams.
In announcing that it would maintain the status quo, CMS said it still has concerns about the quality of clinical evidence backing the utility of CCTA. The agency called for academic societies to develop guidelines that will give healthcare providers more information in determining when CCTA should be used in the diagnostic workup of patients with chest pain.
Learn more about this story by clicking here, or visit our CT Digital Community at ct.auntminnie.com.
Incidental findings on RT planning
In other news, we're featuring a new article in our Radiation Oncology Digital Community on the importance of following up on incidental findings found during CT studies for radiation therapy planning.
The number of suspicious findings that pop up on CT planning scans is typically low, but they do happen, and most radiation oncologists believe that they should be followed up as part of the standard of care. But at the same time, many radiation therapy facilities lack an official policy for routine follow-up.
Should your facility set up such a policy? And to what extent should a diagnostic radiologist be involved in reviewing CT planning studies? Get answers to these questions and more by clicking here, or visit our Radiation Oncology Digital Community at radiation.auntminnie.com.