Thin-section MDCT is more useful than previously thought for identifying patients with pancreatic intraductal papillary mucinous neoplasms (IPMN), a type of neoplasm that is proving to be more dangerous than previously thought.
A new study that compared imaging results to surgical records found that CT accurately identified IPMN features that were associated with both malignancy and parenchymal invasion.
Pancreatic IPMN, defined as intraductal mucin-producing neoplasm with tall, columnar, mucin-containing epithelium, were initially thought to have a favorable prognosis, according to researchers from Nagoya University Graduate School of Medicine in Japan. However, "recent studies have shown a higher rate of invasive carcinoma and a poorer outcome than initially suggested," they wrote. "The presence of parenchymal invasion in IPMN has been reported to be the single strongest adverse predictor of survival," they wrote (Radiology, September 2008, Vol. 248:3, pp. 876-886).
For invasive carcinoma, radical resection with lymph node dissection is generally needed, while limited surgery is sufficient for noninvasive tumors, the researchers explained. Some patients can even be followed without surgery. Therefore, for appropriate triage, "distinguishing among adenoma, noninvasive carcinoma (borderline malignancy and carcinoma in situ), and invasive carcinoma is critical in the treatment of IPMN," they wrote.
Multiphase contrast-enhanced CT with a multisection CT scanner is already known to be useful for identifying which IPMN patients need resection to eliminate the risk of carcinoma, and for surgical planning for IPMN needing resection, wrote study authors Drs. Hiroshi Ogawa, Shigeki Itoh, Mitsuru Ikeda, and colleagues. However, previous studies were lacking with regard to imaging technique, sample size, or statistical analysis of the results.
The retrospective study examined 59 patients (39 men and 20 women; mean age, 64.9 years; range, 41-81 years). A total of 61 tumors were surgically resected with a diagnosis of pathologically confirmed IPMN of the pancreas. Treatment planning was performed prospectively before the patients underwent surgery a mean of 18 days (range, 2-98 days) after imaging with four- (39 tumors) or 16-detector-row (22 tumors) CT imaging (Aquilion, Toshiba, Tokyo).
Based on World Health Organization classifications, surgical specimens were classified into four groups, including findings of adenoma (n = 26), borderline malignancy (n = 5), carcinoma in situ (n = 10), and invasive carcinoma (n = 20).
Patients were given iodinated contrast material (300 mg/mL) at 08. mL per kg of body weight, followed by a 5% dextrose flush, administered by power injector (Auto Enhance A50 and Auto Injector 1205, Nemotokyorindo, Tokyo).
"All images were reconstructed with a 5-mm section thickness at 5-mm intervals," they wrote. "In addition, reconstruction was performed with a 1-mm section thickness at 0.5- or 0.8-mm intervals in all contrast-enhanced images, and multiplanar reformatted images were routinely generated with a 1-mm section thickness at 0.5-mm intervals by radiologic technologists who specialize in three-dimensional imaging."
Two experienced radiologists reviewed the CT images retrospectively and in random order over 10 weeks' time. They were aware of the IPMN diagnosis but unaware of specific findings at surgery, imaging, or pathology. The readers examined all transverse and multiplanar reformatted images reconstructed on the institution's PACS network (RadiForce G20; Eizo, Ishikawa, Japan).
For each lesion, the radiologists assessed the maximum diameter, the presence of a septum, the presence and size of a mural nodule, the type of lesion, and thickened walls. They also looked for abnormal attenuation in the surrounding parenchyma, bile duct dilatation of 10 mm or more. Abnormal attenuating areas were categorized as hypoattenuating, isoattenuating, or hyperattenuating, relative to normal parenchyma.
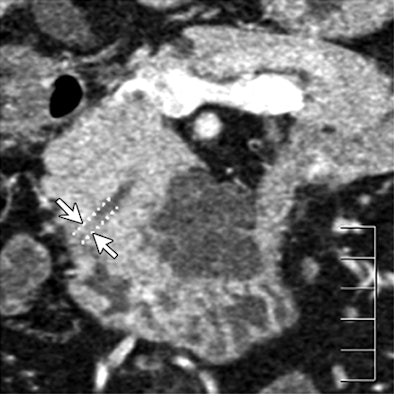 |
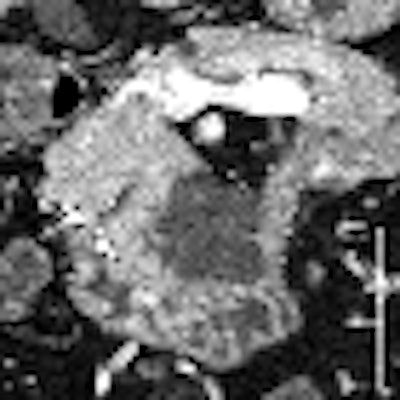
| Dilatation of main pancreatic duct (MPD) in intraductal papillary mucinous neoplasms of the pancreas (IPMN). Oblique coronal reformatted images were generated from pancreatic phase scanning, with 5-cm scale at lower right on each image. Above, adenoma; below, noninvasive carcinoma; bottom, invasive carcinoma. As the maximum diameter of the MPD (arrows indicate distance between dotted lines) increased by 3.8 mm (top), 21.4 mm (below), and 40.9 mm (bottom), the likelihood of malignancy of IPMN increased. Arrowhead on image below indicates protrusion of dilated MPD, showing water attenuation into the ampulla of Vater. Many mural nodules are seen in dilated MPD in invasive carcinoma on bottom image. |
 |
 |
| Images republished with permission of the Radiological Society of North America. Ogawa H, Itoh S, Ikeda M, Suzuki K, Naganawa S, Intraductal papillary mucinous neoplasm of the pancreas: Assessment of the likelihood of invasiveness with multisection CT. Radiology. 2008;248(3):876-886. |
Three or more board-certified pathologists classified the surgical specimens into four groups: adenoma (n = 26), borderline malignancy (n = 5), carcinoma in situ (n = 10), and invasive carcinoma (n = 20). CT findings were compared to pathology results for the presence of adenoma, noninvasive carcinoma, and invasive carcinoma.
The following findings showed significant differences among the three groups: maximum diameter of the main pancreatic duct (MPD), size (length of major axis) of the largest mural nodule in the MPD or in any associated cystic lesion, abnormal attenuating area in the surrounding parenchyma, calcification in the lesion, protrusion of the MPD into the ampulla of Vater, and bile duct dilatation, the authors reported.
Based on these criteria, CT's sensitivity, specificity, and accuracy for the detection of malignancy were 83%, 81%, and 82%, respectively.
"Of seven findings that were significant predictors of invasion in the univariate analysis, the following two findings remained significant in the multivariate analysis: presence of a mural nodule in the MPD of 6.3 mm or larger, and presence of an abnormal attenuating area in the surrounding parenchyma," the authors wrote.
When tumors meeting one or both of these criteria were identified as invasive, CT's sensitivity, specificity, and accuracy for detecting parenchymal invasion were 90%, 88%, and 89%, respectively.
MDCT can distinguish among adenoma, noninvasive carcinoma, and invasive carcinoma in patients with IPMN, the authors concluded. Although previous studies have also found the scans to be useful, several drawbacks including a lack of pancreatic-phase images, multiplanar reconstructions, or logistic regression analysis of the results, rendered them less useful for disease assessment. The present series is also the largest to date, the authors added.
Among the study's new findings was the association of an abnormal attenuating area in the surrounding parenchyma with invasive carcinoma.
"Because this finding showed high sensitivity (80%, 16 of 20) and specificity (90%, 37 of 41) for predicting parenchymal invasion, the presence of an abnormal attenuating area in the surrounding parenchyma should be carefully assessed to avoid missing the parenchymal invasion of IPMN," the authors wrote.
At CT most lesions were seen as hypoattenuating in the pancreatic phase and hyperattenuating in the delayed phase, "a finding that is presumed to be related to the desmoplastic changes associated with tumor invasion and/or secondary inflammation," they wrote, adding that more studies are needed to correlate the findings conclusively with histology. "In addition, the optimal combination of contrast-enhanced phases required for identifying abnormal attenuating areas that reflect parenchymal invasion should be determined," they wrote.
As for study limitations, interobserver variability could not be assessed because the images were read in consensus, the authors noted. Also, the value of CT findings for determining resectability and unresectability was not evaluated. Previous studies have demonstrated that the presence of inflammatory changes such as pancreatitis, "classic criteria for vascular invasion and infiltration of the retroperitoneal fat," have led to overestimation of surgical unresectability at CT, they noted.
"Multiphase contrast-enhanced CT with a multisection CT scanner is helpful for distinguishing among adenoma, noninvasive carcinoma, and invasive carcinoma in patients with IPMN, and such a distinction provides valuable information to assist the clinician in guiding patient treatment," Ogawa and colleagues concluded.
By Eric Barnes
AuntMinnie.com staff writer
August 20, 2008
Related Reading
Adjuvant chemoradiotherapy may improve survival in pancreatic cancer, August 13, 2008
CT rules out malignancy in most pancreatic cysts, June 9, 2008
Survival benefit seen with radiation therapy in early pancreatic cancer, February 6, 2008
CTA of the pancreas reduces failed resections, December 25, 2007
MDCT's 'virtual Whipple' offers practice run before complex surgery, August 16, 2007
Copyright © 2008 AuntMinnie.com