Intravenous tissue plasminogen activator (tPA) works better and is harmful to fewer patients than most doctors think, and, in any case, stroke treatment shouldn't be denied just because CT perfusion says the ischemic area is to large, according to a presentation earlier this month at the International Symposium on Multidetector-Row CT in San Francisco
In a wide-ranging talk on patient selection for ischemic stroke treatment with an emphasis on CT, Dr. Michael Lev spoke about how technology and recent studies continue to alter the decision-making process regarding whether or not patients can be safely treated with IV-tPA or intra-arterial clot-retrieval techniques.
"Perfusion imaging is great, but you should not use it to exclude patients from thrombolysis because perfusion does not measure [the infarct] core," said Lev, who is director of emergency neuroradiology at Massachusetts General Hospital (MGH) and a professor of radiology at Harvard Medical School.
To treat or not to treat?
Whether or not to administer the treatment is a key decision that must be made quickly when stroke patients present to the emergency room.
Radiologists are looking for treatment-relevant acute imaging targets (TRAITs) to inform their choice. Fortunately, CT can identify a number of targets that are gaining in prominence, though diffusion-weighted MRI (DWI-MRI) remains the gold standard for deciding treatment eligibility.
The first question isn't about the effectiveness of the treatment, it's about safety, Lev noted. It's about quantifying the risks versus the benefits of treatment in a way that offers the best chance of recovery without harming the patient.
"We get an unenhanced CT, and if the patient is within three to 4.5 hours of stroke onset, they're otherwise IV-tPA eligible, and there's no bleed, they get IV-tPA," he said. It takes about eight to 10 minutes to mix up the tPA formula -- just about enough time to get a CT angiography (CTA) scan, which serves up two important pieces of information.
"It tells us if there is an occlusion in the M1 or M2 or basilar arteries that is a target for intra-arterial clot retrieval, and it also tells us about the collaterals and how the patient is likely to do if we don't treat them," Lev said.
In the interest of reducing time to treatment, MGH doctors forego CT perfusion if they think someone is a candidate for tPA, and the patient goes straight to DWI-MRI.
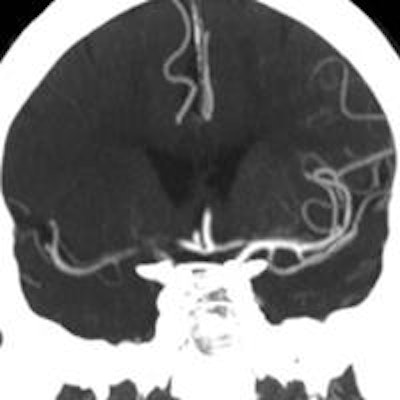
 An ischemic stroke patient with a 1-cm hyperdense vessel at CT angiography (not seen) and no visible collateral vessels (above) was visiting a hospital when the stroke occurred. His proximity led to rapid assessment with CT/CTA within 25 minutes, and IV-tPA initiation within an hour of symptom onset. CT showed an M1 vessel occlusion, and CTA revealed a zero collateral pattern, suggesting a large ischemic area. Early treatment was successful, and follow-up CT shows nearly 100% revascularization. Image courtesy of Dr. Michael Lev.
An ischemic stroke patient with a 1-cm hyperdense vessel at CT angiography (not seen) and no visible collateral vessels (above) was visiting a hospital when the stroke occurred. His proximity led to rapid assessment with CT/CTA within 25 minutes, and IV-tPA initiation within an hour of symptom onset. CT showed an M1 vessel occlusion, and CTA revealed a zero collateral pattern, suggesting a large ischemic area. Early treatment was successful, and follow-up CT shows nearly 100% revascularization. Image courtesy of Dr. Michael Lev.Intra-arterial catheter-based reperfusion
If IV-tPA use doesn't seem appropriate, physicians may decide to treat the clot with intra-arterial therapy (IAT) via catheter-based reperfusion or clot retrieval. The viability of IAT depends on size, Lev explained; multiple studies have found that patients with infarcts larger than 70 mL (length x width x height x 2) have poor outcomes. In fact, a DWI core larger than 70 mL is one of the strongest imaging biomarkers for poor stroke outcome, he said.
"If you have a big infarct at admission, you're going to have a poor outcome anyway," he said. "Most of those people we do not want to risk getting a hemorrhage, and we won't bring them to intra-arterial clot lysis."
At MGH, where the doctors are fortunate enough to have an MRI scanner about 30 ft from the CT scanner, patients amenable to MRI get their DWI perfusion scan right away, and the treatment decision can be based on infarct size as noted above.
Patients with contraindications to MRI go to CT perfusion. Those with occlusions of the internal carotid artery (ICA), middle cerebral artery (MCA), or basilar artery plus a small diffusion lesion are candidates for intra-arterial clot retrieval.
"The reasoning behind our algorithm is that there are only two critical pieces of information: How big is the infarct core, and is there an occlusion amenable to the intra-arterial clot retrieval?" Lev said.
When CT is the tool
Many centers lack available MRI scanners, of course, and many patients have contraindications to the modality, leaving the medical team without DWI-based infarct size assessment, Lev said. In that case, "let me tell you this: IV-tPA works a lot better than we think," he said, citing three major studies that showed its superiority to intra-arterial therapy in almost all cases.
For example, the 2013 Screening Technology and Outcome Project in Stroke (STOP Stroke) study by Gonzalez and colleagues showed good outcomes post-tPA compared to intra-arterial therapy in 649 of the very sickest stroke patients with distal or proximal ICA occlusions.
"When we gave those patients IV-tPA, 35% of them had a good outcome -- that is a great, great result!" Lev said. Conversely, among the patients who didn't get IV-tPA and had an MCA occlusion and similar bad clinical exam at admission, only 17% had positive outcomes (modified Rankin scale ≤ 2).
Dense vessel sign a winner for CT
The dense vessel sign -- really a hyperdense "dot" in the proximal and middle cerebral arteries -- has been in the literature for years. However, a 2011 study by Riedel et al and follow-up work by Dr. Albert Yu, Lev, and colleagues in Massachusetts has renewed interest in its utility by specifically tying dense vessel length to patient outcomes.
"In the setting of hemiparesis and acute stroke symptoms, this dense vessel sign is almost as specific as getting a CTA," Lev said. "If you see it, there's going to be a vessel occlusion there." It works for the basilar artery, as well for patients with a specific history, he added.
"If you do thin-slice CT and you measure the length of the dense vessel, it is an outstanding biomarker for IV-tPA futility," Lev said. "Any [hyperdense vessel] over 8 mm and certainly any one over 1 cm in the MCA has almost a 0% chance of responding to IV-tPA alone. So if you see a dense vessel on your unenhanced CT that's over 1 cm and you have the capability to do intra-arterial therapy, those patients should get it."
The dense vessel sign is also visible on MRI fluid-attenuated inversion recovery (FLAIR) and gradient-echo (GRE) sequences, and it works so well it's even part of the inclusion criteria for the newest Penumbra (Norton Healthcare) reperfusion catheter trial, he said.
CT/CTA collateral mismatch as DWI surrogate
Can CT/CTA substitute for DWI-MRI in assessing infarct volumes? Maybe, according to Lev.
There is a study underway to look at FLAIR/DWI mismatch in the setting of wake-up strokes for which time from symptom onset is unknown. The hypothesis is that if FLAIR is normal but DWI is abnormal, it may be safe to give tPA even without knowing the symptom onset time, Lev said.
The point is not that FLAIR/DWI mismatch is a surrogate for time after event of greater than six hours, he said. Rather, when those sequences reveal a lack of vasogenic edema, it's a biomarker for treatment safety.
A large infarct "where you see vasogenic edema on the FLAIR, where you see a big hypodensity on the CT ... means you already have blood-brain barrier breakdown ... and if you reopen that vessel, the risk of reperfusion hemorrhage is nontrivial," Lev said.
But beware of false positives before declaring a malignant collateral pattern on CTA in a patient with a large hypodense region, Lev said, because calling such a pattern when the patient doesn't really have one could cause treatment to be denied unnecessarily.
"And what we actually found in the study was that the best [CTA] correlation with DWI was only in the zero collateral pattern," meaning a complete absence of collateral vessels on the delayed-enhancement images only. Be sure before foregoing treatment based on CT, he said.
CTP alone for IV-tenecteplase treatment
A 2012 study by Parsons and colleagues found that CT perfusion alone was sufficient for patient selection with IV-tenecteplase; however, there were concerns that the delays involved in waiting for the results might slow or deny treatment for some patients, Lev said.
Still, physicians should never let perfusion imaging unnecessarily slow or deny treatment. Neither CT nor MR perfusion are real substitutes for DWI when it's available, he said.