Isolation protocols implemented to curb the spread of SARS-CoV-2 over the past year have had an unfortunate effect: an increase in rates of intimate partner violence (IPV), which is defined as actions between partners that inflict physical, psychological, or sexual harm, according to a paper published on October 6 in European Radiology.
A team of researchers led by Simon Matoori, PhD, of Harvard University in Cambridge, MA, says that radiologists have an important role to play in identifying victims of partner violence and steering them toward supportive resources.
"The COVID-19 pandemic led to a marked increase in the number of intimate partner violence (IPV) cases, potentially leading to increased emergency department visits and radiological examinations," the authors wrote. "We believe that as radiologists, we can make a difference by being cognizant of this condition, raising an alert when appropriate and treating suspected victims with care and empathy."
Although effective for curbing the spread of SARS-CoV-2, stay-at-home orders have exacerbated existing mental and physical health challenges for many people, in part due to an inability to access support services -- prompting an increase in intimate partner violence, Matoori and colleagues noted.
Most conditions related to intimate partner violence are fractures in the face (48.3%), fingers (9.9%), or upper trunk (9.8%), and it can be easy to interpret them as routine trauma, according to the authors. That's why radiologists should thoroughly review the medical history of cases that are suspicious for domestic abuse, discuss these cases with the referring physician, and conduct a private conversation with the patient, educating them on available resources for victims, the authors wrote.
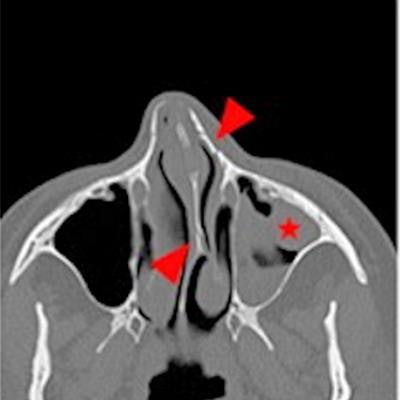
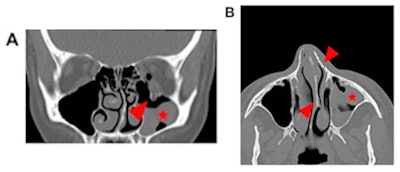 Case 1: A 42-year-old female presenting with diplopia after she reported having been punched by her partner in the face. Head CT revealed a left orbital floor fracture (arrowhead, A), blood-filled left maxillary sinus (asterisk, A, B), and nasal bone fractures as well as a nasal septum fracture (arrowhead, B) with deviation of the nasal septum to the left (arrowhead, B). The patient initially reported that she had run into a cupboard. Careful questioning indicated that she was attacked by her life partner. A social worker and, later, the police were informed. Images and caption courtesy of European Radiology.
Case 1: A 42-year-old female presenting with diplopia after she reported having been punched by her partner in the face. Head CT revealed a left orbital floor fracture (arrowhead, A), blood-filled left maxillary sinus (asterisk, A, B), and nasal bone fractures as well as a nasal septum fracture (arrowhead, B) with deviation of the nasal septum to the left (arrowhead, B). The patient initially reported that she had run into a cupboard. Careful questioning indicated that she was attacked by her life partner. A social worker and, later, the police were informed. Images and caption courtesy of European Radiology.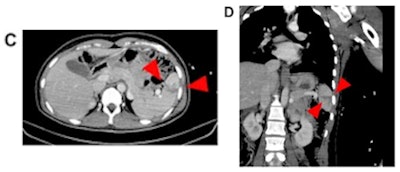 Case 2: After reporting a blunt trauma to the abdomen by her partner, abdominal CT of a 41-year-old female revealed splenic injury with parenchymal laceration (arrowheads) without intra-abdominal bleeding (C, D). The injury was treated conservatively and regularly checked by ultrasound. The bleeding stopped spontaneously. Police were informed.
Case 2: After reporting a blunt trauma to the abdomen by her partner, abdominal CT of a 41-year-old female revealed splenic injury with parenchymal laceration (arrowheads) without intra-abdominal bleeding (C, D). The injury was treated conservatively and regularly checked by ultrasound. The bleeding stopped spontaneously. Police were informed.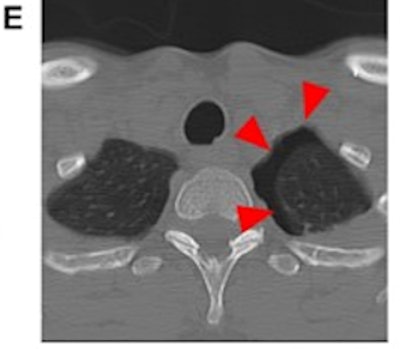 Case 3: A 49-year-old female patient was suspected to have been pushed by her partner, resulting in a fall against a bathtub. Caudal slices of a cervical spine CT showed incidental traumatic pneumothorax on the left side (arrowheads) as a result of rib fractures (not illustrated), but no pathology of the cervical spine (E). The police were informed. IPV was self-reported after questioning by medical professionals in these cases; however, we have no information on the outcomes of the police investigations on the alleged attacks.
Case 3: A 49-year-old female patient was suspected to have been pushed by her partner, resulting in a fall against a bathtub. Caudal slices of a cervical spine CT showed incidental traumatic pneumothorax on the left side (arrowheads) as a result of rib fractures (not illustrated), but no pathology of the cervical spine (E). The police were informed. IPV was self-reported after questioning by medical professionals in these cases; however, we have no information on the outcomes of the police investigations on the alleged attacks.Matoori and colleagues acknowledged that talking to suspected victims of intimate partner violence can be challenging. They proposed a three-part protocol:
- Communicate first with referring physicians or care team when intimate partner violence is suspected. There may already be information about the patient's situation in the medical record.
- Create a safe and private space to discuss domestic abuse with the patient. "Even if the abuser is not present, the relationship of the accompanying person to the abuser may impede the patient from disclosing any information," the team noted.
- Inform patients that healthcare providers are required to maintain confidentiality and that no information will be shared beyond the medical team or recorded in the medical record against the patient's preference. But also be clear about state/country policies regarding the obligation to report intimate partner violence to appropriate entities. Offer the patient resource information such as emergency services, hospital programs, and domestic abuse support groups.
Cases of intimate partner violence offer radiologists an opportunity to further participate in the continuum of care, according to Matoori's team.
"As radiologists move beyond the reading room and join the multidisciplinary team providing direct care to the patient, they may choose to volunteer to handle IPV cases, especially if they are trained to handle the complexities of these conversations," the researchers concluded. "Indeed, radiologists and radiographers are uniquely positioned to engage with IPV victims due to the physical separation between the victim and any accompanying persons in the radiology department."





















