Although use of CT colonography (CTC) for colorectal cancer screening doubled between 2019 and 2021, overall utilization may still be low, according to research published in the September edition of Clinical Imaging. Upcoming Medicare reimbursement may change that.
In an analysis of CTC use among 58,058 adults in the National Health Interview Survey from 2010 through 2021, researchers from the University of Texas Southwestern Medical Center found that utilization was similar between 2010 (1.3%) and 2019 (1.4%) for adults aged 50 to 75. However, use increased to 3.5% in 2021, a statistically significant increase (p < 0.05). Overall, 1.7% of adults indicated they had received CTC across all of the years in the study.
After performing multivariable analysis, the researchers also found that CTC use was associated among Hispanic patients (odds ratio = 1.73), non-Hispanic Black patients, (odds ratio = 2.07), household income less than 200% of federal poverty level (odds ratio 1.25 vs. > 400% of federal poverty level). What’s more, adults with a history of diabetes (odds ratio = 1.2), chronic obstructive pulmonary disease (odds ratio = 1.58), cancer (odds ratio = 1.29), or past-year hospital admissions (odds ratio = 1.44) were also more likely to receive CTC.
"Our findings suggest that CTC may be an integral part of strategies to increase uptake of and reduce well-documented disparities in CRC screening," wrote medical student Ali Abbas, Cecilia Brewington, MD, and colleagues in that article.
Gaining momentum
CTC, also known as virtual colonoscopy, appears poised to get a boost from the recent proposal by the U.S. Centers for Medicare and Medicaid Services (CMS) to receive Medicare reimbursement beginning in 2025.
Although many private insurers have already been covering CTC, more may begin advocating its use for colorectal cancer screening now that the procedure has gotten a green light for Medicare coverage, according to American College of Radiology (ACR) Colon Cancer Committee Chair Judy Yee, MD.
For AuntMinnie.com, Yee explained what made the difference for the 2024 decision, the hurdles that remain for screening CT colonography, and what radiologists can expect from reimbursement.
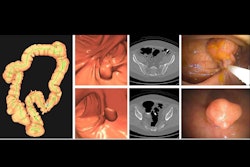
In the eyes of the U.S. Preventive Services Task Force (USPSTF), screening CT colonography has been a valid screening test since 2016, a decision USPSTF reaffirmed in 2021. Other societies such as the American Cancer Society affirmed CTC years ago as CTC is a noninvasive way to provide structural views of the colon and rectum. However, some authorities held out, and the CT-based screening exam traveled a rocky road.
ACR lobbied the issue with CMS for over 15 years. The Harvey L. Neiman Health Policy Institute (HPI) studied screening CTC too, finding that Medicare coverage of screening CTC could potentially reduce income-based disparities for individuals avoiding optical colonoscopy due to invasiveness, need for anesthesia, complication risk, or time away from work. A 2023 article penned by Neiman Research Director Eric Christensen, PhD, for the American Roentgen Ray Society, noted that approximately one-third of the eligible U.S. population have not undergone guideline-compliant CRC screening.
Tests such as stool DNA, fecal immunochemical, flexible sigmoidoscopy, and colonoscopy received Medicare reimbursement sooner than screening CTC, noted Yee, a well-known CTC researcher, educator, and advocate who also serves as professor and university chair of radiology at the Albert Einstein College of Medicine and Montefiore Medical Center in New York.
"The body of peer-reviewed literature out there about CTC was much larger than for many of the other tests," Yee continued. "The largest payers in this country already reimbursed for screening CTC, but a lot of people don't know about it.
"In the long run, if you prevent patients from developing colorectal cancer, there are significant savings in not requiring surgery, chemotherapy, and radiation therapy -- so that the test pays for itself," Yee said. "We've made quite a bit of headway in that diagnostic CTC has been reimbursed, and gastroenterologists have had the chance to understand what the test is about and what we can do.
"We would love to bring in many more patients for screening and to send to colonoscopy those patients who are most likely to have a true polyp, that our gastroenterologist colleagues can then resect, perform polypectomy, and prevent cancers from occurring,” Yee added. “We know that it is a struggle to bring patients in for colorectal cancer screening. The needle has moved up a bit in terms of new patients coming in for screening, but it has stagnated and plateaued off."
Colorectal cancer is the leading cause of cancer death in men under 50 in the U.S., and the burden of disease is higher for Black Americans, who are more than 20% more likely to get colorectal cancer and 40% more likely to die of it compared with their white or Hispanic peers, according to the American Cancer Society.
With the announcement of Medicare coverage for screening CTC in its 2025 Hospital Outpatient Prospective Payment System (HOPPS) and 2025 Medicare Physician Fee Schedule (MPFS) proposed rules, CMS said CTC would replace colorectal cancer screening using barium enema, a test used only limited circumstances and usually not for colorectal cancer screening, Yee said.
3 questions
What happened in 2024 that played the biggest role in CMS changing its position on CT colonography for colorectal cancer screening? Yee explained in the video below.
Do any hurdles remain for screening CT colonography?
What is the reimbursement for CTC? Plus, using computer-aided detection.
"CMS has proposed that screening CTC be subject to the Deficit Reduction Act payment cap, meaning that office-based technical component reimbursement will be at the lesser of the OPPS or MPFS reimbursement rate," explained ACR's Senior Director of Economic Policy Katie Keysor in an email. "While the [relative value units] RVUs for screening CTC in the MPFS are good, the proposed OPPS payment rate is approximately $106, so this rate will apply in both the hospital outpatient and physician office settings. The professional component is $104 in both settings.
"We are currently comparing these numbers to reimbursement for other colorectal cancer screening tests," Keysor noted. "We recognize that low reimbursement for CTC may deter providers from offering it, so this will be something we address in our comments to CMS."
Availability gaps
Research has shown that Medicare fee-for-service beneficiaries who reside in communities with annual per capita income of $100,000 or more are 5.7 times more likely to receive CTC than their counterparts residing in communities with per capita income of less than $25,000, according to HPI. In addition, the ACR My CT Colonography Screening Location Finder map shows low availability in some states around the U.S.
"Encouraging facilities to register is something we have focused on during colorectal cancer awareness month, and we will continue to do so moving forward, particularly if/when Medicare coverage if finalized," Keysor added, noting that the registry is voluntary. The ACR Colon Cancer Committee has also had discussions about increasing opportunities for physician training on CTC and making sure CTC is available in underserved communities.
"These will be focus areas once the coverage proposal is finalized by CMS," Keysor said.
The ACR offers a CTC Registry Startup Guide and more about practice parameters on its NRDR Support hub.