Photon-counting CT may serve as an alternative to MRI for assessing liver fat in patients with fatty liver disease, according to an article published September 24 in Radiology.
A team led by Huimin Lin, MD, of Shanghai Jiao Tong University in China, tested the technique in a large group of patients enrolled in a clinical trial and found it matched the overall performance of MRI proton density fat fraction, the current most accurate method.
“This study validated the use of photon-counting detector CT for accurate, protocol-independent liver fat quantification in metabolic dysfunction-associated steatotic liver disease across various imaging settings,” the group wrote.
Accurate quantification of liver fat is an essential prerequisite for treatment and follow-up of metabolic dysfunction-associated steatotic liver disease (MASLD), the authors explained. The disease affects up to 24% of the population in the U.S. and can lead to cirrhosis and even cancer if left untreated.
Although MRI has been established as a noninvasive imaging approach for liver fat assessment, patients are required to hold their breath for 20 seconds during image acquisition, which can lead to poor image quality, and MRI is not possible in patients with metal implants or claustrophobia, the researchers explained.
Conversely, photon-counting CT has several purported benefits, including improved spatial resolution and spectral separation, and it has shown promise for quantifying liver fat in early studies, even in patients with obesity. Yet more robust studies are needed to further validate the technology, they wrote.
To that end, between September 2023 and March 2024, the researchers enrolled 412 asymptomatic participants and 122 participants with MASLD. They compared “fat fractions” derived from photon-counting CT versus MRI. All patient underwent both scans within one month. Participants were randomly assigned to six groups with different CT protocols regarding tube voltage (90, 120, or 140 kVp) and radiation dose (standard or low).
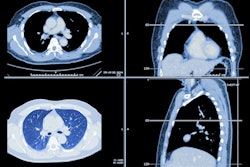
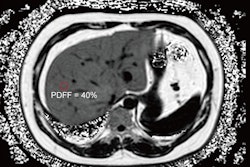
 Liver fat content measurement with photon-counting CT and MRI-based proton density fat fraction (PDFF). Three regions of interest (circles) were delineated in the peripheral areas of the left, right anterior, and right posterior lobes of the liver. (A) Representative axial unenhanced 120-kVp standard-dose CT image (left) and corresponding MRI scan (right) in a 33-year-old man (body mass index, 26.2) diagnosed with metabolic dysfunction-associated steatotic liver disease (MASLD) in the asymptomatic cohort. (B) Representative axial unenhanced 120-kVp low-dose CT image (left) and corresponding MRI scan (right) in a 69-year-old woman (body mass index, 24.6) in the MASLD cohort. Body mass index was calculated as weight in kilograms divided by height in meters squared.Image courtesy of the RSNA.
Liver fat content measurement with photon-counting CT and MRI-based proton density fat fraction (PDFF). Three regions of interest (circles) were delineated in the peripheral areas of the left, right anterior, and right posterior lobes of the liver. (A) Representative axial unenhanced 120-kVp standard-dose CT image (left) and corresponding MRI scan (right) in a 33-year-old man (body mass index, 26.2) diagnosed with metabolic dysfunction-associated steatotic liver disease (MASLD) in the asymptomatic cohort. (B) Representative axial unenhanced 120-kVp low-dose CT image (left) and corresponding MRI scan (right) in a 69-year-old woman (body mass index, 24.6) in the MASLD cohort. Body mass index was calculated as weight in kilograms divided by height in meters squared.Image courtesy of the RSNA.
According to the findings, across all comparisons in asymptomatic patients, photon-counting CT fat fractions (CTFF) demonstrated excellent agreement with MRI proton density fat fractions (PDFF) (mean bias values < 1%). In addition, CTFF error was not influenced by tube voltage, radiation dose, or body mass index. Agreement between CTFF and PDFF was also found in the MASLD cohort (mean bias, −0.2%).
“Standardized CT value from [photon-counting] CT showed a robust and remarkable agreement with MRI PDFF across various protocols and may serve as a precise alternative for liver fat quantification,” the group wrote.
In an accompanying editorial, Benjamin Wildman-Tobriner, MD, of Duke University Medical in Durham, NC, described the study as “well executed and encouraging.”
“As [photon-counting] CT continues to become more prevalent, we may one day see it used for routine liver quantification tasks,” he wrote.
However, Wildman-Tobriner noted a limitation, that the study was conducted using one vendor’s photon-counting CT system (Naeotom Alpha VA50, Siemens Healthineers). Additional vendors’ versions of the technology are currently being made available, and harmonization across platforms will be important, he wrote.
“Future studies addressing this issue will become feasible as additional scanners are installed across radiology departments,” Wildman-Tobriner concluded.
The full study is available here.