Radiologists play a crucial role in the care of patients with Marfan syndrome, a systemic connective tissue disorder with life-threatening cardiovascular implications.
Radiologists allow for early identification and confirmation of clinical suspicion and/or careful observation of patients with this potentially lethal condition. Given the broad spectrum of manifestations, many of which are evident on imaging, radiologists and cardiologists are often the first to recognize the constellation of findings that suggest Marfan syndrome. Early recognition by radiologists can lead to timely diagnosis and intervention, potentially preventing serious complications such as aortic dissection or sudden cardiac death.
Beyond initial detection, radiologists contribute to patient management by providing precise and reproducible measurements -- especially critical in evaluating aortic root dilation. Cross-sectional imaging allows radiologists to measure the aorta orthogonal to its true axis, a technique essential for avoiding over- or underestimation of dilation. Their expertise also aids in distinguishing Marfan syndrome from phenotypically similar conditions such as Loeys-Dietz syndrome or Ehlers-Danlos syndrome, which carry different prognoses and management pathways.
What is Marfan syndrome?
Marfan syndrome is an autosomal dominant connective tissue disorder caused by mutations in the FBN1 gene, which encodes fibrillin-1, a glycoprotein essential for the integrity of elastic fibers. The syndrome affects multiple organ systems, most notably the cardiovascular, ocular, and skeletal systems. Clinical manifestations are variable but commonly include aortic aneurysms, ectopia lentis, and skeletal overgrowth. The estimated prevalence is approximately one in 5,000 individuals, although the condition is likely underdiagnosed.
Diagnosis is based on the revised Ghent nosology, which incorporates clinical findings, family history, and molecular testing. Imaging plays a pivotal role both in the initial evaluation and in the long-term surveillance of affected individuals. While echocardiography is often the first imaging modality used to assess the aortic root, cross-sectional imaging -- such as CT or MRI -- is crucial for confirming measurements.
Such imaging becomes imperative for patients with suboptimal echocardiographic windows due to thoracic wall deformities. Furthermore, full-body cross-sectional imaging may be warranted to assess the entire aorta and its branches for aneurysmal disease or dissection. Rarely, previously undiagnosed patients may present with an acute aortic syndrome. Knowing the imaging findings allows for the diagnosis of Marfan syndrome to be made clinically so that postoperative care can be optimized.
Imaging findings of Marfan syndrome
Aortic
One of the hallmark features of Marfan syndrome is progressive dilation of the aortic root, particularly at the sinuses of Valsalva (also known as annuloaortic ectasia). This dilatation results in the characteristic light bulb shape of the aorta seen in patients with Marfan syndrome. This predisposes patients to life-threatening complications such as aortic aneurysm, dissection, and rupture.
Aortic root dilation. Radiologically, aortic root dilation is typically the earliest and most critical finding. Diagnostic thresholds are generally set at greater than 40 mm for younger male patients and greater than 37 mm for younger female patients. These measurements must be made in a plane orthogonal to the axis of the aortic root to ensure accuracy. Measurements should be performed bidirectionally (as opposed to the cusp to commissure tridirectional measurement used with transcatheter valve planning) to mirror those obtained on echocardiography and studied in the literature.
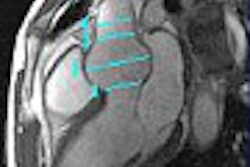
 A 33-year-old man with Marfan syndrome and dilated aortic root. On the transverse images (A) the aorta measures 4.5 cm by 4.2 cm. When corrected for long axis (B) of the aorta, the aorta measures 3.9 cm by 4.2 cm. Measurements obtained orthogonal to the long axis of the aorta allow for consistent sizing and accurate risk assessment. Volume rendered image shows the root dilatation with mild effacement of the sinotubular junction (see below). This phenotype is sometimes referred to as annuloaortic ectasia, a characteristic finding of Marfan syndrome. Additional axial and coronal images of aortic dilation are provided (see below). All images courtesy of Sanjeev Bhalla, MD, and Mensur Koso, MD.
A 33-year-old man with Marfan syndrome and dilated aortic root. On the transverse images (A) the aorta measures 4.5 cm by 4.2 cm. When corrected for long axis (B) of the aorta, the aorta measures 3.9 cm by 4.2 cm. Measurements obtained orthogonal to the long axis of the aorta allow for consistent sizing and accurate risk assessment. Volume rendered image shows the root dilatation with mild effacement of the sinotubular junction (see below). This phenotype is sometimes referred to as annuloaortic ectasia, a characteristic finding of Marfan syndrome. Additional axial and coronal images of aortic dilation are provided (see below). All images courtesy of Sanjeev Bhalla, MD, and Mensur Koso, MD.


Tortuous arteries. Arterial tortuosity, particularly in the cervical and cerebral vasculature, may also be noted and is sometimes more characteristic of Loeys-Dietz syndrome, especially in the head and neck region, though it can appear in Marfan patients as well.
Cardiac
Mitral valve prolapse. Mitral valve abnormalities, especially mitral valve prolapse (MVP), are common. Imaging reveals thickened or elongated leaflets (indicative of myxoid degeneration), often accompanied by mitral regurgitation. These findings can be assessed via echocardiography and, when needed, further confirmed with cardiac MRI.
 A 39-year-old woman with Marfan syndrome. Thickening of the mitral valve is in keeping with myxoid degeneration. Focal dissection of the descending aorta is also seen.
A 39-year-old woman with Marfan syndrome. Thickening of the mitral valve is in keeping with myxoid degeneration. Focal dissection of the descending aorta is also seen.
Aortic valve regurgitation. Aortic regurgitation may result from annular dilation or abnormalities of the aortic valve.
Thoracic
Pectus excavatum. This chest wall deformity, characterized by a concave depression of the sternum, is frequently observed. While not specific to Marfan syndrome, it contributes to the overall clinical picture and may affect echocardiographic imaging quality.
 Severe pectus excavatum in a 24-year-old man with Marfan syndrome post ascending aortic repair.
Severe pectus excavatum in a 24-year-old man with Marfan syndrome post ascending aortic repair.
Pulmonary diseases. One of the more characteristic pulmonary imaging findings is the so-called "tulip bulb" configuration of the upper lungs. This refers to a subtle widening of the upper lobe apices with concave tapering inferiorly on frontal chest radiographs or coronal CT images. It is thought to be related to upper lobe emphysematous changes or apical pleural blebs. These structural abnormalities, along with an increased incidence of spontaneous pneumothorax, are important to recognize, particularly in younger patients presenting with acute chest pain and no trauma history. In rare cases, restrictive lung disease may result from severe scoliosis or pectus excavatum, contributing to impaired pulmonary mechanics.
 30-year-old man with biapical blebs and a history of Marfan syndrome. CR image shows the classic tulip bulb shape of Marfan syndrome.
30-year-old man with biapical blebs and a history of Marfan syndrome. CR image shows the classic tulip bulb shape of Marfan syndrome.
Skeletal
Skeletal overgrowth. Patients often present with tall stature, disproportionately long limbs (dolichostenomelia), and long fingers and toes (arachnodactyly). These features, although clinically evident, are often also seen incidentally on radiographic studies.
 19-year-old man with foot findings that can be seen with Marfan syndrome including arachnodactyly and pes planus.
19-year-old man with foot findings that can be seen with Marfan syndrome including arachnodactyly and pes planus.
Scoliosis. Spinal curvature is common and may be severe, warranting imaging for evaluation and monitoring.
 A 34-year-old man being followed after aortic repair. Cinematic rendering shows the marked scoliosis form a posterior view.
A 34-year-old man being followed after aortic repair. Cinematic rendering shows the marked scoliosis form a posterior view.
Dural ectasia. One of the most specific skeletal findings is lumbosacral dural ectasia, a ballooning or widening of the dural sac. It is best visualized on MRI of the lumbosacral spine and is considered a major diagnostic criterion in the revised Ghent nosology.

 Same 39-year-old woman from above. More inferiorly dural ectasia can be seen with posterior scalloping of the sacrum typical of Marfan syndrome.
Same 39-year-old woman from above. More inferiorly dural ectasia can be seen with posterior scalloping of the sacrum typical of Marfan syndrome.
Ophthalmic
Ectopia lentis. Dislocation of the ocular lens, typically superotemporal, is a classic feature. While this is primarily diagnosed by ophthalmologic examination, orbital imaging may incidentally reveal lens displacement.
High myopia: Severe nearsightedness is another common ocular finding.
The takeaway
 Sanjeev Bhalla, MD.
Sanjeev Bhalla, MD.
Radiologists are uniquely positioned to identify the hallmark features of Marfan syndrome and should maintain a high index of suspicion when encountering compatible findings across various imaging modalities. Early and accurate identification by radiologists can significantly impact patient outcomes by prompting timely referral and appropriate surveillance.
 Mensur Koso, MD.
Mensur Koso, MD.
Marfan syndrome is a systemic condition with genetic roots and multisystem involvement, including characteristic cardiovascular, musculoskeletal, and ocular manifestations. High-yield imaging findings include aortic root dilation, mitral valve prolapse, thoracic cage deformities, dural ectasia, and ectopia lentis.
Given their integral role in diagnosis and management, radiologists must be familiar with the imaging spectrum of Marfan syndrome, recognize its mimics, and provide detailed, accurate assessments to guide clinical decision-making.
Sanjeev Bhalla, MD, is a professor of radiology at the Mallinckrodt Institute of Radiology at Washington University School of Medicine in St. Louis. He is the current section chief of cardiothoracic imaging and vice chair of education.
Mensur Koso, MD, is an incoming radiology resident at the Mallinckrodt Institute of Radiology at Washington University in St. Louis. His interests include cardiothoracic and abdominal imaging, interventional radiology, nuclear medicine, and artificial intelligence.
The comments and observations expressed herein are those of the authors and do not necessarily reflect the opinions of AuntMinnie.com.