Flexible positioning markers may be more accurate than adhesive markers when scaling for digital templating before total hip arthroplasty (THA), according to a study presented at the 2008 American Academy of Orthopaedic Surgeons (AAOS) meeting in San Francisco.
Orthopedic surgeons traditionally have planned hip surgeries using templates of orthopedic implant hardware that are manually overlaid on hard-copy films, typically anteroposterior pelvis radiographs and lateral views of the hip. The arrival of digital x-ray and PACS has made this job much easier, however, as digital hardware templates can now be inserted directly into images on a workstation. As a result, the use of traditional plain-film radiography is rapidly declining for orthopedic applications.
But there are still challenges to digital templating. Digital images can vary in magnification due to several factors, ranging from patient obesity to differences in the positioning techniques of radiologic technologists, and this can affect the accuracy of digital templating. Previous research has shown that preoperative assessments based on templating could be 18% inaccurate, and this inaccuracy can increase the likelihood that an improper implant could be chosen.
One way to compensate for magnification differences is to place a marker of a predetermined size into the x-ray field along with the patient, giving orthopedic surgeons a sense of the scale of the template relative to the rest of the digital image. This is believed to improve the likelihood that the correct orthopedic implant is chosen, but until now no research has been done on the accuracy of markers based on position, according to the authors of the study presented at the AAOS show.
In the study, the researchers examined a group of 106 patients who had undergone THA surgery to assess the accuracy of two of the most widely used x-ray markers in digital templating. One marker uses a flexible ball/stick design (OrthoMark, RolleSolutions, Castro Valley, CA), while the other employs an adhesive ball design (X-Marker, Eisenlohr Technologies, Davis, CA).
Researchers were able to achieve the most accurate position on digital x-rays -- at the level of the greater trochanter -- with 68% of flexible ball/stick markers. However, almost 4% of adhesive ball markers ended up at this most accurate position on the x-ray, and 73.2% were pictured at the least accurate position with bony overlap.
"Preoperative templating is critical to the accuracy of total hip arthroplasty. So the message is not to give up on templating, but to note the position of each marker in order to calculate accuracy, and use flexible markers whenever possible," said Christopher Bayne, a medical student at Harvard Medical School in Boston.
The researchers noted that preoperative templating before THA has many benefits, including accurately predicting prosthetic size, reducing intraoperative complications, and achieving appropriate off-set and leg-length equality.
In fact, the study was designed by Dr. Thomas Barber, associate physician in chief at Kaiser Permanente in Oakland, after a problem case in which a patient was fitted with a prosthesis that was the wrong size during a THA, and ended up with a leg-length discrepancy. The problem arose because x-rays were taken in one facility, and printed at another -- as a result, the templates came up with the wrong size, Barber said.
"Magnification markers are critical to sizing (prostheses) for THA. And, in fact, leg-length discrepancy after THA is one of the most litigated issues in the U.S. By carefully templating cases, you can avoid these problems," he said. "But knowing the magnification factor in advance is quite important."
The difficulties of digital scaling are twofold: objects must be placed at the same level within the x-ray field and at the same distance from the emission source to experience the same magnification. Also, the accuracy of measurements based on scaling can vary greatly depending on the marker location.
In the study, the frequency of correct versus incorrect marker placement was calculated for both types of markers. Four positions were assessed:
- The correct placement (A) at the level of the greater trochanter
- A second position (B) with soft-tissue overlap of the marker
- A third position (C) with bony overlap of the marker
- A fourth position (D) (the second most accurate) in which there was no contact between the marker and soft tissue
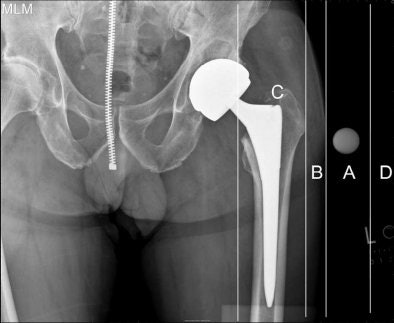 |
| Digital hip image above demonstrates four possible positions for x-ray templating markers. Markers placed in the area represented by position A, at level of the greater trochanter, proved to be the most accurate, according to the authors. Image courtesy of Dr. Thomas Barber. |
Templating measurements were performed by one investigator for all x-rays. The same radiographs were evaluated a second time after three weeks by a different investigator who was blinded to the results of the first investigator. Marker accuracy was calculated based on position, and the estimated measurements were compared to actual measurements to calculate accuracy.
The researchers found that the flexible-positioning marker was easier to place accurately because of its ability to rigidly maintain its position in space. The adhesive marker also had to be attached to soft tissue, and could not be applied with pressure. As a result, more potential space could be between the marker and the greater trochanter, with more variability in position.
"If the patient moved or rotated the leg, and the marker shifted, then it is no longer an accurate reflection of the magnification," Barber said.
If an x-ray does show soft-tissue or bony overlap, there's likely an error in magnification, and that error is related to how much overlap there is, he said. "So you may have to shoot the x-ray again. These days with digital x-ray, we're highly reliant on magnification," Barber said.
By Barbara Boughton
AuntMinnie.com contributing writer
March 31, 2008
Related Reading
PACS offers direct access to MSK specialists without alienating rads, October 18, 2007
Radiation oncology and PACS: ramping up for the digital age, August 9, 2007
MRI, CT prove their metal for imaging orthopedic hardware, May 4, 2007
X-ray planning improves hip replacement surgical outcomes, January 18, 2006
Ortho group stumbles with DR, completes conversion to digital CR, May 27, 2005
Copyright © 2008 AuntMinnie.com