VIENNA - MRI outperforms PET in predicting myocardial recovery following coronary artery bypass grafting (CABG), according to research presented at this week’s European Congress of Radiology. MRI’s higher specificity and positive predictive value should make it the reference standard for presurgical assessment of CABG according to researchers from University Hospital in Essen, Germany.
"As you know, myocardial viability determines the outcome after coronary revascularization in coronary artery disease," said Dr. Peter Hunold in his presentation. "It’s very important that the (presurgical) test predict the regional recovery of function, and PET today serves as a clinical reference standard in imaging technique of viability. But certainly the real gold standard from the assessment standpoint of recovery after revascularization...is the comparison to the prediction before the surgery."
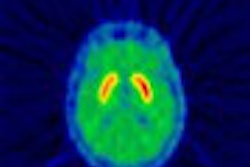
The purpose of the study was to compare contrast-enhanced MRI with FDG-PET for the prediction of functional recovery after revascularization in patients with occlusive coronary artery disease, Hunold said. It was done by performing both PET and MRI in patients presurgically, using the results to predict myocardial recovery, and testing the predictions six months later with MRI.
In the study, 12 male patients with angiographically proven occlusive coronary artery disease underwent MRI of the myocardium on a 1.5-tesla Sonata scanner (Siemens Medical Solutions, Erlangen, Germany) both presurgically and 6 months after CABG. Functional studies of long and contiguous short-axis slices were performed using a TrueFISP sequence (TR/TE 3.0/1.5 ms, FA 60, 8 mm slice thickness).
Then, 8-15 minutes after administration of a double dose of Gd-DPTA contrast (Imagnevist, Schering AG, Berlin), short axes were scanned using a segmented inversion-recovery TurboFLASH sequence (TR/TE 8/4 ms, TI 200-260) in order to detect late enhancement of the myocardium, Hunold said. Patients also underwent standard PET imaging; FDG uptake and MRI results were both evaluated using the same 8-segment model in short axes.
Hunold said the group worked with the hospital’s nuclear medicine department to devise the PET scoring system. "In PET we judged score 1, normal FDG uptake, score 2, decreased FDG uptake but more than 50% of the reference line, until score 4, no FDG uptake," he said. In MRI, a score of 1 meant no enhancement, 2 was the cutoff for 50% enhancement or more, and 4 indicated optimal mural enhancement.
Presurgical MRI was used to judge each segment as norokinetic, hypokinetic, akinetic or dyskinetic; while postsurgical MRI assessed segmental functional improvement, he added.
In all, the group evaluated 1,008 such segments with MRI and PET. Six months after the CABG procedure, 150 of 406 (37%) of the dysfunctional segments improved function. Based on the identification of viable myocardium with functional recovery after revascularization, MRI had a sensitivity and specificity of 95% and 72%, respectively, compared with 97% and 47%, respectively, for PET.
"We had no difficulties in characterizing the improving segments as viable in both techniques, but in PET you can see that more than half (71) of the viable segments (predicted) in PET (143) did not improve after surgery," Hunold said. However, he added that modifying the ROC values used in analysis could change the results.
While negative predictive values were high for both techniques (96% and 97% for MRI and PET, respectively) the positive predictive value was higher for MRI (66%) compared with PET (52%), Hunold said. MRI more reliably detects the scarring that inhibits functional recovery, he said.
"We have seen that MRI more reliably detects scars, and seems to be superior to PET for the prediction of functional recovery," Hunold concluded, adding that more patients will be needed to validate the results.
After the presentation, Hunold was asked to discuss why he thought most of the published literature gives PET the edge in specificity. For one thing, Hunold said, the strict inclusion criteria for his group’s study required 50% stenosis or greater. Moreover, his group’s findings of a 66% positive predictive value for MRI were not spectacular, just a little better than PET’s at 52%.
The cutoff points for viability in PET were another bone of contention. Hunold said his group has worked closely with the nuclear medicine department to design the PET cutoff points, and would continue to assess the study design.
By Eric BarnesAuntMinnie.com staff writer
March 11, 2003
Related Reading
Referring physicians reserve perfusion imaging for sickest patients, September 30, 2002
Real-time MR stress imaging detects cardiac wall-motion abnormalities, September 23, 2002
New tracers, technologies propel clinical applications in PET, June 14, 2002
Copyright © 2003 AuntMinnie.com