Hyperparathyroidism is on the rise. An estimated two in 1,000 American women over age 40 suffer from the disease. In Europe, its prevalence in the general population is estimated at three in 1,000 (Journal of Bone and Mineral Research, November 2002, Vol. 17:11, pp. 2061-2067).
Recently, however, advances in parathyroid imaging have made minimally invasive surgery a viable alternative to conventional surgery; more so in cases in which the condition is caused by a single parathyroid adenoma.
While 99mTc sestamibi imaging is the accepted standard modality, ultrasound, SPECT, CT, MRI, and radionuclide scintigraphy are also used preoperatively. Two recent studies have shed light on parathyroid imaging and minimally invasive radioguided surgery (MIRS) for hyperparathyroidism.
SPECT stands alone
SPECT/CT has no significant clinical value over conventional SPECT for parathyroid imaging except in locating ectopic parathyroid glands, according to research from the University of Texas, M. D. Anderson Cancer Center in Houston.
"Eliminating the CT acquisition will spare patients the additional time, radiation exposure, and expense," concluded Dr. Isis Gayed and co-authors in their retrospective study of 48 patients with a clinical diagnosis of primary hyperparathyroidism (PHPT).
Earlier studies have shown SPECT improves sensitivity and accuracy when used with radionuclide scintigraphy (Journal of Nuclear Medicine, June 2003, Vol. 44:6, pp. 904-908).
In their current findings, Gayed and colleagues noted there was no significant difference in the identification rate of the diseased parathyroid gland with the addition of the CT portion. According to the group, planar and SPECT imaging, with or without CT fusion, identified 89% of the surgically confirmed diseased parathyroid glands in the study population.
Use of SPECT/CT changed the diagnosis in only one patient (2%), and better located the glands in only four patients (8%).
Images were acquired after an intravenous injection of 740-925 MBq of 99mTc sestamibi. Anterior planar images of the neck and chest were obtained immediately and 60 minutes later, using a high-resolution low-energy parallel-hole collimator and large-field-of-view dual-detector gamma camera with a mounted CT scanner.
"SPECT and CT images of the same area were obtained at 30 minutes after injection over a 360-degree arc, using 120 frames at 23 seconds per frame and 3-degree angles. The CT part was acquired at a slice step of 10 mm, a slice time of 14 seconds, a current of 2.5 mA, and a voltage of 140 kV," the group wrote (JNM, February 2005, Vol. 46:2, pp. 248-252).
Two readers who were blinded to the results indicated whether the scan was negative or positive for locating the diseased parathyroid gland after reading the planar images, the planar and SPECT images, and the planar and SPECT/CT images. They noted if SPECT and SPECT/CT interpretation changed the PHPT diagnosis, and the usefulness of SPECT and SPECT/CT in locating the gland.
 |
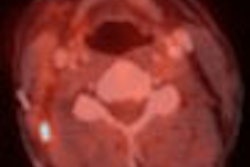
| SPECT/CT accurately located ectopic parathyroid gland behind left sternoclavicular joint. Locating gland helped with planning preoperative parathyroidectomy to minimize dissection. Reprinted with permission from the Society of Nuclear Medicine. Gayed IM; et al, "The Value of 99mTc-Sestamibi SPECT/CT Over Conventional SPECT in the Evaluation of Parathyroid Adenomas or Hyperplasia" (J Nucl Med 2005; 46:248-252, Fig. 2, p. 250). |
Surgery confirmed the positive scan findings. Thirty-two of the patients with positive scan findings underwent surgery, and 35 diseased parathyroid glands were resected. The remaining patients did not undergo surgery because 10 had negative scan findings, two had comorbidity with a primary cancer, one refused surgery, and three were lost to follow-up.
Since all the findings could not be confirmed on surgery, the sensitivity and specificity of SPECT/CT could not be calculated. "Thus, the actual number of false-negatives and true-negatives is unknown. Therefore, we used the term identification rate instead of the term sensitivity to evaluate the accuracy of our imaging method," the group stated.
Among the 48 patients in the cohort, 34 had normal thyroid glands, eight had multinodular glands, four underwent total thyroidectomies, and two had hemithyroidectomies.
Despite some value for locating ectopic parathyroid adenomas, SPECT/CT offered no advantage over SPECT for assessing hyperparathyroidism in general, the authors stated, adding that omitting the CT exam would have saved imaging time and unnecessary radiation exposure.
Identifying patients for MIRS
In a second study, Italian researchers found 99mTc sestamibi scintigraphy combined with neck ultrasonography offered a high degree of accuracy in identifying PHPT patients suitable for MIRS.
Dr. Domenico Rubello led the multi-institutional group of researchers as part of the Italian Study Group on Radioguided Surgery and Immunoscintigraphy (GISCRIS).
They selected candidates with a high likelihood of a solitary parathyroid adenoma for MIRS using preoperative 99mTc sestamibi scintigraphy and ultrasonography from a cohort of 384 consecutive PHTP patients. Patients with multigland disease, nodular goiter, suspicion of malignancy, or negative 99mTc sestamibi findings were excluded. About 70% (277 of 384) of the patients were found suitable.
MIRS was performed using an intraoperative handheld gamma probe, and was successful in 96.8% (268 of 277) of the selected patients. "No major surgical complications were observed in the MIRS group, and there were only 24 cases (11%) of transient postoperative hypocalcemia," the authors wrote (JNM, February 2005, Vol. 46:2, pp. 220-226).
Interestingly, MIRS was also successful in 32 (78%) of 41 patients who had undergone prior thyroid surgery or unsuccessful parathyroid surgery. Prior surgery is usually considered a contraindication for minimally invasive surgery (Surgery, December 2003, Vol. 134:6, pp. 849-857).
For MIRS, the group used a low-dose 99mTc sestamibi different-day protocol. "A different-day protocol appears preferable in geographic areas with a high prevalence of concomitant nodular goiter, and allows better scheduling of daily activity in the operating theatre," the authors explained. The procedure took a mean operating time of 37 minutes and a mean hospital stay of 1.2 days. Locoregional anaesthesia was used in 72 patients.
99mTc sestamibi (37-110 MBq, or 1-3 mCi) was injected 10-30 minutes before the start of the intervention. The gamma probe was used externally to identify the area with the maximum count activity, and a 2- to 2.5-cm surgical incision was made in the midline of the neck or lateral neck.
The gamma probe was inserted through the incision to guide the surgeon to the area with maximum count activity or the parathyroid adenoma. The gamma probe measured the radioactivity count rate on the parathyroid adenoma, thyroid gland, and thyroid background, as well as the ex-vivo parathyroid adenoma to check for the success of the procedure. The researchers used surgical bed gamma-probe scanning to verify the completeness of tissue removal.
Intraoperative quick parathyroid hormone (IQPTH) assay was used in 308 patients, and was useful in detecting some cases of multigland parathyroid disease.
"Reduction in IQPTH levels to less than 50% of the baseline preoperative values 10 minutes after removal of a parathyroid adenoma indicated successful removal of all hyperfunctioning parathyroid tissue. When IQPTH did not decrease by more than 50%, multigland disease was suspected and surgery was extended to explore other possible sites of (parathyroid adenoma)," the researchers explained.
Four of the patients selected for MIRS were converted to bilateral neck exploration because IQPTH levels continued to be high even after the preoperatively visualized parathyroid adenoma was removed. Five others were converted to bilateral neck exploration because of an intraoperative frozen-section diagnosis of parathyroid carcinoma, or the parathyroid adenoma was difficult to remove.
Based on the success rate in the patient group selected for MIRS, the surgery "plays a limited role in patients with concomitant 99mTc sestamibi-avid thyroid nodules, and should be discouraged in patients with negative 99mTc sestamibi findings preoperatively," the group concluded.
By N. Shivapriya
AuntMinnie.com contributing writer
April 7, 2005
Related Reading
Lemon candy may suck for curbing dry mouth after thyroid cancer therapy, March 2, 2005
Hypothyroidism tied to reduced breast cancer risk, February 15, 2005
Ultrasound aids congenital hypothyroidism diagnosis, November 29, 2004
Copyright © 2005 AuntMinnie.com