PET imaging can help guide treatment decisions in children with brain tumors when cranial MRI exams fail to provide clinicians with enough information, according to a research team in Germany.
Investigators at the University of Augsburg studied the impact of PET imaging with an amino acid radiotracer (F-18 FET) in pediatric patients with newly diagnosed and previously treated central nervous system (CNS) tumors. In cases where cranial MRI exams failed to provide enough detail, FET-PET scans guided treatment in more than half of the patients, they found.
"F-18 FET-PET is a robust imaging tool, which provides important additional information for treatment decisions in pediatric and adolescent patients with CNS tumors, especially in clinically challenging situations," wrote first author Dr. Olivia Kertels. The study was published January 21 in the European Journal of Nuclear Medicine and Molecular Imaging.
Primary CNS tumors are the most common solid malignancies and one of the main causes for cancer-related deaths in children, with a five-year overall survival rate of up to 75%. Cranial MRI is the standard imaging approach for both adults and children, and FET-PET is an established tool in adult brain tumor imaging. Yet few studies are available on the use and utility of FET-PET in pediatric brain tumors, according to the authors.
To that end, the researchers analyzed the impact of FET-PET in children in a real-world clinical scenario -- namely, in complex cases at their hospital in which insufficient information had been gained from cranial MRI exams.
The group analyzed outcomes in 21 consecutive pediatric and adolescent patients with primary CNS tumors who underwent FET-PET for further diagnostic work-up between July 2010 and October 2018. Two nuclear medicine physicians studied the impact on clinical decision-making due to addition of FET-PET.
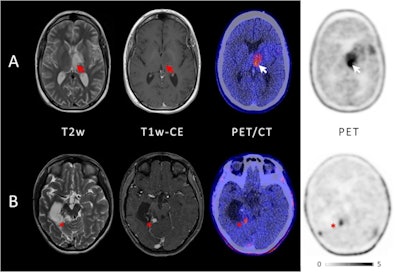 Example of two patients with concordant imaging results (A) and incremental diagnostic value of F-18 FET-PET (B). (A) Example of a patient with an anaplastic astrocytoma WHO grade III who was treated with combined radiochemotherapy prior to PET. Axial T2-weighted imaging and T1-weighted imaging with contrast enhancement depict the tumor in the left thalamus and insular region (red arrows); axial PET shows high uptake of F-18 FET in these regions (white arrows). Both MRI and PET correctly identified the tumor recurrence. (B) Example of a patient with a pilocytic astrocytoma who was treated with surgery and chemotherapy prior to PET. Axial T2-weighted imaging and T1-weighted imaging with contrast enhancement show cystic as well as contrast-enhancing lesions next to the surgical cavity consistent with both unspecific changes and tumor recurrence (red asterisk); in contrast, axial PET demonstrates focal high uptake of F-18 FET (white asterisk). Image courtesy of the European Journal of Nuclear Medicine and Molecular Imaging through CC BY 4.0.
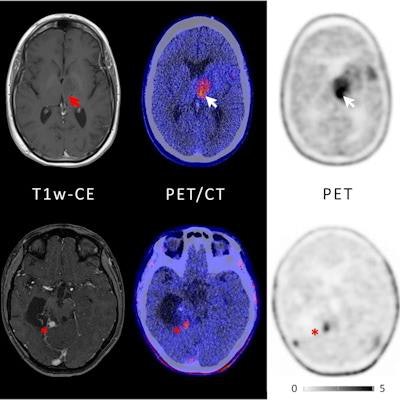
Example of two patients with concordant imaging results (A) and incremental diagnostic value of F-18 FET-PET (B). (A) Example of a patient with an anaplastic astrocytoma WHO grade III who was treated with combined radiochemotherapy prior to PET. Axial T2-weighted imaging and T1-weighted imaging with contrast enhancement depict the tumor in the left thalamus and insular region (red arrows); axial PET shows high uptake of F-18 FET in these regions (white arrows). Both MRI and PET correctly identified the tumor recurrence. (B) Example of a patient with a pilocytic astrocytoma who was treated with surgery and chemotherapy prior to PET. Axial T2-weighted imaging and T1-weighted imaging with contrast enhancement show cystic as well as contrast-enhancing lesions next to the surgical cavity consistent with both unspecific changes and tumor recurrence (red asterisk); in contrast, axial PET demonstrates focal high uptake of F-18 FET (white asterisk). Image courtesy of the European Journal of Nuclear Medicine and Molecular Imaging through CC BY 4.0.Fourteen out of the 21 patients showed positive uptake of the FET radiotracer by tumors: three out of five with newly diagnosed brain tumors and 11 out of 16 with previously treated lesions. In these patients, FET-PET had an impact on further treatment decisions, the researchers found.
Specifically, invasive surgery or biopsy was avoided in four patients, and PET was crucial to biopsy or surgery guidance in another four patients. In three patients, FET-PET directly changed further therapy: One patient received chemotherapy instead of radiotherapy, chemotherapy was changed to another regimen in another patient, and one patient received no further radiotherapy. In one patient, FET-PET confirmed a suspicion of true tumor progression and prompted subsequent surgery.
"Our real-world data suggest that F-18 FET-PET is a useful adjunct in challenging pediatric settings," the authors concluded.





















