F-18 FDG-PET/CT scans may help predict relapses in patients with autoimmune pancreatitis, according to a study published January 17 in BMC Gastroenterology.
In an analysis of F-18 FDG-PET/CT scans in patients with autoimmune pancreatitis (AIP) prior to treatment, specific imaging findings were higher in a group that subsequently relapsed than in those who did not relapse, noted first authors Shengxin Chen and Guanyun Wang, of Chinese PLA General Hospital in Beijing, and colleagues.
“Relapse seriously affects the lives of patients and comprises a heavy psychological burden; therefore, it is necessary to identify predictors of relapse during clinical diagnosis and treatment,” the group wrote.
AIP is a rare form of chronic pancreatitis first described in 1995, the authors explained. The clinical profile of AIP includes enlargement of the pancreas, irregular narrowing of the pancreatic duct, and the involvement of multiple organs.
While patients respond well to treatment with corticosteroids, relapse rates may be as high as 60% and there is no definite consensus regarding the predictive factors in these cases, they added.
To that end, the group explored the use of F-18 FDG-PET/CT. They noted that the technique is used to evaluate involved organs, lesion severity, and to monitor AIP patient responses to treatment, yet its predictive value for AIP relapse is unknown.
Out of 103 consecutive patients with AIP who underwent F-18 FDG PET/CT before treatment, they included a cohort comprised 51 patients (37 males and 14 females) with a mean age of 62.7 years (±11.8 years); 33 of these patients experienced relapse and 18 did not.
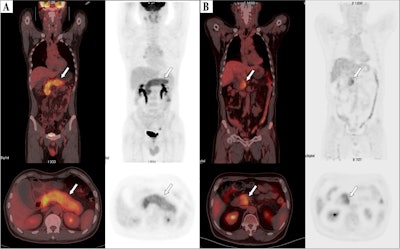 F-18 FDG-PET/CT images of patients. (A) Image of a 61-year-old male patient with type 1 autoimmune pancreatitis (AIP) demonstrating diffuse enlargement of the pancreas (arrows). The serum IgG4 level was 2,260.0 mg/dL, and the TLG2.5 was 413.8 g/ml×cm3. According to the nomogram, his relapse probability is more than 95%. The patient discontinued steroid use during the maintenance phase, and 7 months later, he relapsed, with imaging showing diffuse re-enlargement of the pancreas. (B) Image of a 60-year-old male patient with type 1 AIP, showing focal enlargement in the head of the pancreas (arrows). The serum IgG4 level was 980 mg/dL, and the TLG2.5 was 92.7.0 g/ml×cm3. According to the nomogram, the patient’s relapse probability is less than 50%. After symptom relief, the patient did not receive maintenance treatment, and has been followed up for 4 years without relapse. Image courtesy of BMC Gastroenterology.
F-18 FDG-PET/CT images of patients. (A) Image of a 61-year-old male patient with type 1 autoimmune pancreatitis (AIP) demonstrating diffuse enlargement of the pancreas (arrows). The serum IgG4 level was 2,260.0 mg/dL, and the TLG2.5 was 413.8 g/ml×cm3. According to the nomogram, his relapse probability is more than 95%. The patient discontinued steroid use during the maintenance phase, and 7 months later, he relapsed, with imaging showing diffuse re-enlargement of the pancreas. (B) Image of a 60-year-old male patient with type 1 AIP, showing focal enlargement in the head of the pancreas (arrows). The serum IgG4 level was 980 mg/dL, and the TLG2.5 was 92.7.0 g/ml×cm3. According to the nomogram, the patient’s relapse probability is less than 50%. After symptom relief, the patient did not receive maintenance treatment, and has been followed up for 4 years without relapse. Image courtesy of BMC Gastroenterology.
In a univariable analysis, the relapsed group showed higher levels of F-18 FDG radiotracer uptake in affected areas. Specifically, maximum standardized uptake value (SUVmax) (6 vs. 5.2, p = 0.047), standardized uptake value ratio (SUVR) (2.3 vs. 2; p = 0.026), and total lesion glycolysis (234.5 vs. 139.6; p = 0.02) were all higher among relapsed patients, they wrote.
Moreover, a predictive model based on these parameters demonstrated an area under the curve of 0.806, they wrote.
“We found that pretreatment F-18 FDG PET/CT metabolic parameters may be useful predictors of relapse,” the group wrote.
Ultimately, the group noted that to the best of their knowledge, this is the first study to explore F-18 FDG-PET/CT metabolic parameters to predict AIP relapse. As such, its generalizability is limited, they noted.
“Given the rarity of AIP and limited sample size, we were only able to perform internal validation, which nevertheless yielded promising results,” the group concluded.
The full study can be found here.