A PET/MRI study has provided insights into the neurobiology of late-life depression, with researchers reporting that tau protein – a key protein involved in Alzheimer’s disease – does not appear to be involved in the condition.
The finding comes from a group at the Leuven Brain Institute in Leuven, Belgium, who compared tau PET/MRI brain scans among participants with late-life depression, mild cognitive impairment (MCI) due to Alzheimer’s disease, and nondepressed older adults.
“Understanding this is of particular importance in clinic practice as it could provide clinicians treating older adults with potential biomarkers for differential diagnosis of MCI and primary major depressive disorder,” noted lead author Thomas Vande Casteele, MD, and colleagues. The study was published July 18 in the American Journal of Geriatric Psychiatry.
Late-life depression is a major depressive disorder that affects up to 10% of adults over the age of 60 years old, according to the authors. Besides depressed mood, these patients are often affected by cognitive impairment and are more at risk of developing Alzheimer's disease, they noted.
Moreover, neuroimaging studies in diagnosed patients consistently show lower gray-matter volume compared to non-depressed cognitively unimpaired participants in regions typically involved in Alzheimer’s disease, they added. Still, it is not clear whether lower gray-matter volume in these patients is related to the pathological processes underpinning Alzheimer’s disease – specifically, beta-amyloid plaque deposits and neurofibrillary tau tangles, according to the authors.
To explore this issue, the researchers enrolled 19 currently depressed participants diagnosed with late-life depression, 19 participants with MCI due to Alzheimer’s disease, and 36 nondepressed cognitively unimpaired participants. All patients were of similar ages and all were white.
As part of previous studies, participants had undergone PET/MRI scans, 3D T1-weighted structural MRI to derive grey-matter volume (GMV) in seven brain regions (temporal, cingulate, prefrontal, and parietal regions), amyloid PET scans to assess amyloid positivity, and neuropsychological tests.
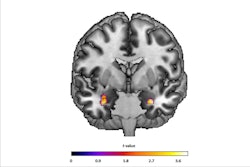
![Coronal and axial slice of the average cortical F-18 MK-6240 SUVR [standard uptake value ratio] image for each study population. SUVR images were corrected for partial volume effects and masked with the gray matter mask used for volume of interest delineation. Overall tau accumulation is comparable between the late-life depression (LLD, middle column) and non-depressed cognitively unimpaired comparison (HC, left column) groups, while abnormal tau accumulation, which is most pronounced in the mesial temporal lobe, can be seen in the mild cognitive impairment due to Alzheimer's disease group (right column). Image and caption courtesy of the American Journal of Geriatric Psychiatry.](https://img.auntminnie.com/files/base/smg/all/image/2024/07/Tau_depressed.66a16540ee0a1.png?auto=format%2Ccompress&fit=max&q=70&w=400) Coronal and axial slice of the average cortical F-18 MK-6240 SUVR [standard uptake value ratio] image for each study population. SUVR images were corrected for partial volume effects and masked with the gray matter mask used for volume of interest delineation. Overall tau accumulation is comparable between the late-life depression (LLD, middle column) and non-depressed cognitively unimpaired comparison (HC, left column) groups, while abnormal tau accumulation, which is most pronounced in the mesial temporal lobe, can be seen in the mild cognitive impairment due to Alzheimer's disease group (right column). Image and caption courtesy of the American Journal of Geriatric Psychiatry.
Coronal and axial slice of the average cortical F-18 MK-6240 SUVR [standard uptake value ratio] image for each study population. SUVR images were corrected for partial volume effects and masked with the gray matter mask used for volume of interest delineation. Overall tau accumulation is comparable between the late-life depression (LLD, middle column) and non-depressed cognitively unimpaired comparison (HC, left column) groups, while abnormal tau accumulation, which is most pronounced in the mesial temporal lobe, can be seen in the mild cognitive impairment due to Alzheimer's disease group (right column). Image and caption courtesy of the American Journal of Geriatric Psychiatry.
According to the findings, compared to non-depressed participants, late-life depression patients showed lower GMV in temporal and anterior cingulate regions, but similar tau accumulation and amyloid positivity rates.
In contrast, MCI patients had significantly higher tau accumulation in all regions. Moreover, tau did not correlate with any neuropsychological test scores in late-life depression patients, the researchers wrote.
“Our findings suggest [Alzheimer's disease]-type tau is not higher in [late life depression] compared to non-depressed, cognitively unimpaired older adults and appears unlikely to contribute to lower gray matter volume in LLD,” the authors wrote.
Ultimately, the results further underscore the need to distinguish major depressive disorder from depressive symptoms occurring in early Alzheimer’s disease, the researcher wrote. However, further studies are needed to determine if tau PET scans could help play a role, they noted.
“Whether tau imaging can increase diagnostic accuracy in differentiating [late life depression] from early stages of [Alzheimer’s disease] remains to be shown,” the group concluded.
The full study is available here.