Using PET/MRI rather than standard imaging could significantly improve the diagnosis, treatment, and overall outcomes for patients with rectal cancer, researchers have reported.
The finding is from a comparison among 42 patients who underwent initial clinical staging with CT and/or MRI and were then restaged with whole-body F-18 FDG PET/MRI, noted lead author Rafał Maksim, MD, of the Maria Skłodowska-Curie National Research Institute of Oncology in Warsaw, Poland.
“F-18 FDG-PET/MR demonstrates significant value in the preoperative staging of rectal cancer, with our study providing evidence for its diagnostic superiority in detecting lymph node involvement and tumor deposits compared to standard imaging techniques,” the group wrote. The study was published September 12 in the International Journal of Colorectal Disease.
Mortality rates are rising in rectal cancer, particularly among younger adults under 50 years old, the authors noted. In 2025, approximately 154,270 cases are projected to be diagnosed in the U.S., resulting in approximately 52,900 deaths, they wrote.
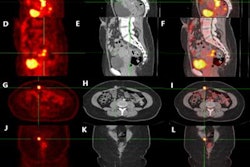
Hybrid PET/MRI is an innovative diagnostic tool that combines anatomical information from multiparametric MRI of the pelvis and precise metabolic information from PET, yet the data on its use in staging rectal cancer is scarce, the researchers added.
To bridge the knowledge gap, the group compared PET/MRI to standard imaging regarding clinical stage assessment, dimensions, lymph nodes, and tumor deposits in the mesorectum.
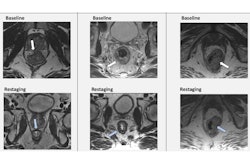
The researchers recruited 42 patients with histologically confirmed rectal cancer. After standard initial clinical staging with CT and/or MRI, all patients were scheduled for preoperative radiotherapy or radiochemotherapy. Before the treatment, all patients were restaged with whole-body, F-18 FDG-PET/MRI (Biograph mMR, Siemens Healthineers).
According to the results, F-18 FDG-PET/MRI provided superior detection of lymph nodes and tumor deposits, with the highest diagnostic accuracy for tumor length measurement (area under the receiver operating characteristic curve [AUC] = 0.73; p < 0.05). A model that combined maximum standard uptake value for lymph nodes and carcinoembryonic antigen (blood test) values achieved an AUC of 0.921 (p < 0.001).
In addition, in 11 cases, PET/MRI led to an upstage; in 16 cases, it resulted in a downstage; and in 15 cases, the clinical stage remained unchanged, the researchers reported.
“Our results show that PET/MR changed the clinical stage in 64% of the patients and altered clinical management in 26%, confirming that PET/MRI is functional in restaging [rectal cancer] patients,” the group wrote.
While the results are promising and support the integration of PET/MRI into clinical pathways for rectal cancer assessment, the authors noted the limitations of the small cohort size.
"Further validation through larger multicenter prospective studies and longitudinal evaluation of patient outcomes is essential to establish robust diagnostic thresholds and determine the full clinical value of this imaging approach," the researchers concluded.
The full study is available here.