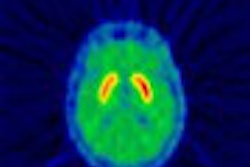
Dopamine transporter imaging using 123I beta-CIT SPECT may improve the accuracy of Parkinsonian syndrome diagnosis, according to a report from the American Academy of Neurology (AAN) meeting last week in Honolulu.
Dr. Danna Jennings and colleagues at the Institute for Neurodegenerative Disorders in New Haven, CT, assessed the usefulness of this modality in 35 patients who had been referred by their community-based neurologist with a diagnosis of suspected Parkinsonian syndrome.
"Because Parkinsonian syndrome remains a clinical diagnosis, several diagnoses are commonly mistaken for early Parkinsonian syndrome," said Jennings, director of clinical research. "These include essential tremor, vascular Parkinsonism, drug-induced Parkinsonism, Alzheimer’s disease, and aging. An accurate diagnosis would aid in appropriate treatment and would also ensure more appropriate recruitment of patients for clinical studies."
Recent studies involving subjects with early Parkinson’s disease indicate that a number of individuals enrolled in clinical trials may have extrapyramidal symptoms, but do not have a dopamine transporter deficit, she continued. 123I beta-CIT SPECT provides a reliable measure of striatal dopamine transporter density and may be used to monitor disease progression.
In the study, the community neurologists provided their best-guess diagnosis before referral, classifying patients as either having Parkinsonian syndrome or not having Parkinsonian syndrome.
Patients then underwent imaging with 123I beta-CIT and SPECT and were assigned an imaging diagnosis based on visual and quantitative analysis. A follow-up clinical examination was performed at six months by one of the movement disorders experts, who remained blinded to the imaging data in order to establish a final diagnosis. The final clinical diagnosis was considered the gold standard for the trial.
Results showed disagreement between the community neurologist and the gold standard diagnosis in 25% of cases, between the movement disorders experts and the gold standard in 20%, and between the imaging diagnosis and the gold standard in 6%. Eight subjects diagnosed with Parkinsonian syndrome by the community neurologist were diagnosed as not having Parkinsonian syndrome by the gold standard.
In all cases where a Parkinsonian syndrome diagnosis was made according to the SPECT exam, agreement with the gold-standard diagnosis was achieved. SPECT missed two out of 12 cases of Parkinsonian syndrome.
In the final clinical exam, the following alternative diagnoses were given: essential tremor, vascular Parkinson’s disease, psychogenic Parkinsonism, drug-induced Parkinsonism, and no neurologic disease.
Overall, the results showed that imaging at baseline improved diagnostic accuracy when compared to the clinical diagnosis made by a referral physician and the movement disorders expert, Jennings said. She added that future studies should increase sample size, extend follow-up to 12 months, and examine patients earlier in the course of disease (i.e., with symptoms present for less than two years).
By Jill SteinAuntMinnie.com contributing writer
April 7, 2003
Related Reading
PET makes progress in documenting movement disorders, March 4, 2003
MRI advances diagnosis of Hallervorden-Spatz syndrome, January 29, 2003
Imaging agent aids diagnosis of Parkinson’s, December 4, 2002
New tracers, technologies propel clinical applications in PET, June 14, 2002
Copyright © 2003 AuntMinnie.com