For nearly a decade, beginning with an unexpected trend among arthritis sufferers, epidemiological studies have found that regular use of non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, appears to stave off Alzheimer’s disease.
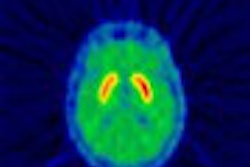
Now, molecular imaging has enabled researchers to see for the first time how NSAIDs appear to prevent and even dissolve the amyloid plaque brain lesions that characterize, and likely cause, Alzheimer’s disease. The breakthrough finding, reported in the March issue of Neuroscience, gives direction for drug development and greater impetus for imaging that identifies the plaques before they cause irreversible cell damage in the brain.
"This really changes the perspective, because right now there are no drugs that are modifying the course of the disease in any way," said principal investigator Jorge Barrio, Ph.D., a professor in the nuclear medicine division, department of molecular and medical pharmacology, David Geffen School of Medicine at UCLA in Los Angeles.
"Now for the first time we have an opportunity to really understand how to proceed with drugs that modify the course of the disease," Barrio said. "This is going to be helpful to patients at risk, people who have a history of Alzheimer’s disease, and even people with very, very early symptoms."
In the UCLA group’s latest study, post-mortem tissue slices from a 79-year-old woman with definitive Alzheimer’s disease were pretreated with NSAID solutions and a chemical marker developed by the UCLA researchers, a hydrophobic radiofluorinated molecular imaging probe called 18FFDDNP.
The group has previously used the radiolabeled marker to image amyloid plaques in Alzheimer’s patients and control subjects. ("PET scanning plus new molecular probe detects early Alzheimer's disease in vivo".;)
In the latest study, the investigators then used digital autoradiography, exposing the specimens to β+ -sensitive phosphor plates for 40 minutes and then scanning them with a BAS 5000 Phosphorimager (Fujifilm Medical Systems USA, Stamford, CT). They also performed fluorescence microscopy of the samples to observe the concentration-dependent decreases in the FDDNP binding to senile plaques, in the presence of some NSAIDs. Additional in vitro research showed the anti-aggregation or plaque-dissolving effects of these NSAIDs (Neuroscience, March 2003, Vol. 117:3, pp. 723-730).
Interestingly, the plaque-binding and anti-aggregation effects were seen with (S)-naproxen and (R)- and (S)-ibuprofen, but not with diclofenac. The lack of competitive binding by diclofenac may suggest other binding sites for that drug or may be consistent with its postulated mode of action of mitigating the neurotoxic inflammatory response in Alzheimer’s disease, the authors wrote.
The most important finding of the in vitro research, Barrio said, was that ibuprofen and naproxen are directly interacting with the amyloid plaques. The next step will be to look for the same interaction in vivo; Barrio expects to begin a new study examining living subjects with 18FFDDNP-PET in the new few weeks.
The PET imaging could be useful for further explaining the effects seen in vitro, and for evaluating the efficacy of select NSAIDs as anti-aggregation agents. But although Barrio is already pursuing the greater potential of 18FFDDNP as an investigational device with the FDA, any prospect for routine clinical use of 18FFDDNP-PET to identify Alzheimer’s in early stages is years away.
The long timeline is an inherent aspect of research involving Alzheimer’s disease, Barrio wrote, because there is no gold standard for diagnosing the disease until autopsy. Therefore, any device that purports to detect Alzheimer’s early on will only be validated, at the earliest, as those patients develop symptoms such as mild cognitive impairment.
"The clinical diagnosis becomes a little more accurate when the symptoms become obvious," Barrio noted. "But at that time, the patient is history. There’s nothing you can do."
"Early diagnosis without a therapeutic outcome, in my book, is not really a desirable goal in itself," Barrio added. He said he would like to see his research help pharmaceutical companies develop new drugs that exhibit the preventative effects of NSAIDs without the secondary effects of gastrointestinal bleeding that currently preclude many people from using them.
Barrio also said he would like to see 18FFDDNP develop into a screening tool within his lifetime.
"My hope is that we could do with Alzheimer’s disease the same thing we are doing with cancer or cardiovascular disease," he explained. "We have mammography for breast cancer, we have colonoscopies for colorectal cancer, we have treadmills for cardiovascular disease. Why not look at Alzheimer’s disease in the same way? Why wait for the clinical symptoms?"
By Tracie L. ThompsonAuntMinnie.com contributing writer
April 8, 2003
Related Reading
FDG-PET spies early decline in forgetful folks, October 10, 2002
PET scanning plus new molecular probe detects early Alzheimer's disease in vivo, January 10, 2002
Using PET for Alzheimer's diagnosis lowers cost of care, October 21, 2002
New PET radiotracer could replace FDG for detecting Alzheimer’s, March 26, 2001
Copyright © 2003 AuntMinnie.com