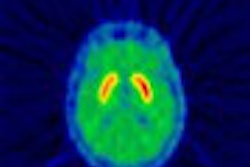
Brain perfusion SPECT can detect abnormalities in patients with spinal multiple sclerosis (MS) and other inflammatory or demyelinating diseases involving the spinal cord, researchers said at the 2003 American Academy of Neurology meeting in Honolulu.
Dr. Bianca Weinstock-Guttman and colleagues with the State University of New York in Buffalo found that, in many instances, the SPECT exam identified problems in patients who had normal MR exams.
"Although MRI detects white matter lesions of MS within the brain with a high sensitivity, about 10% of patients will have normal brain MRI scans," she explained. "The diagnostic confirmation in these patients may require multiple repeated tests."
Their radiotracer of choice was 99mTc-Bicisate ethyl cysteinate dimmer (Neurolite, Bristol-Myers Squibb Medical Imaging, North Billerica, MA). Using SPECT, they compared the characteristics in MS patients presenting with predominantly spinal cord involvement to other spinal cord demyelinating entities, including neuromyelitis optica and isolated transverse myelitis.
Results showed that patients with spinal cord demyelinating processes with normal brain MRI results actually have abnormal brain hypoperfusion on SPECT. This finding suggests that the disease process is more disseminated than is shown on brain MRI, said Weinstock-Guttman, who is director of the Comprehensive Baird MS Center at the university.
The trial included eight patients with MS, three with neuromyelitis optica, and four patients with isolated transverse myelitis. All of the patients had myelopathy, according to clinical exam and MR, but still had normal brain MRI results.
Their mean age was 48.1, disease duration was 5.26 years, and the Expanded Disability Status Scale (EDSS) score was 3.58.
All of the test reports were initially read by one experienced observer. An independent blind reader re-evaluated the SPECT scans in order to confirm the findings. The hypoperfusion abnormalities were rated mild to severe and ranked on a scale from 0 to 5.
SPECT studies were abnormal in all patients due to patchy, widespread heterogeneous hypoperfusion changes affecting the cortex and white matter, with the most constant reduction being seen in the frontal area, according to Weinstock-Guttman.
Significant correlation was found between EDSS and hypoperfusion severity (p=0.0053). However, no clear differences were seen on SPECT abnormalities between isolated transverse myelitis and MS after correction for disease duration. Patients with neuromyelitis optica frequently had abnormal occipital perfusion with or without abnormal visual evoked potentials or visual clinical abnormalities.
This gray matter hypometabolism worsened over time on the SPECT studies, but the T2-weighted MR hyperintensities remained stable. In addition, SPECT-HMPAO studies in MS patients showed frontal gray matter hypoperfusion that was significantly correlated with neurological and cognitive disability.
Defining an abnormal hypoperfusion pattern in the brain of MS patients in the absence of visualized lesions in the routine MRI image may allow the development of a diagnostic and prognostic tool for tracking disease progression, Weinstock-Guttman said. The SPECT analysis may also help better elucidate the complex MS pathophysiology, including effects on gray matter, she added.
Recent data using other imaging techniques such as MR spectroscopy, magnetization transfer resonance, and FDG-PET suggest a more global involvement of the brain than indicated by standard MRI techniques, she said. FDG-PET studies have demonstrated that MS patients had widespread hypometabolism, including cortical and subcortical gray matter that correlated with brain atrophy.
By Jill SteinAuntMinnie.com contributing writer
April 24, 2003
Related Reading
Doppler ultrasound keeps an eye on optic neuritis, March 28, 2003
MRI findings may predict long-term multiple sclerosis disability, January 17, 2002
Dedicated brain market opens new door for SPECT scanner, March 13, 2001
Copyright © 2003 AuntMinnie.com