
Fever of unknown origin (FUO) can be notoriously difficult to diagnose. According to the Petersdorf criteria, FUO is defined as "more than three weeks of illness with fever higher than 38.3° C documented on several occasions and no diagnostic clues despite one week of intensive patient investigation" (Journal of Nuclear Medicine, February 2002, Vol. 43:2, pp.140-144).
As a result, pinpointing the characteristics and parameters of FUO is time-consuming and potentially costly. With regard to imaging, the foci of long-standing fevers can elude standard imaging modalities such as CT and MR.
But molecular imaging may solve the FUO mystery. German and Dutch investigators turned to FDG-PET for FUO, while a group from Denmark relied on 111In-granulocyte scintigraphy in the hopes of finding the optimal diagnostic tool.
Finding the foci
In a presentation at the 2003 Society of Nuclear Medicine conference in New Orleans, Dr. Stefan Dresel discussed his team’s work with hybrid FDG-PET. Dresel is from the University of Munich.
"FUO presents a diagnostic and therapeutic dilemma. Other modalities did not solve the problem of finding the foci responsible for the symptoms," Dresel said. "The results (in our study) were compared with lab findings, MRI, CT, and bone scans. The FDG-PET findings were either confirmed with follow-up or through surgical intervention."
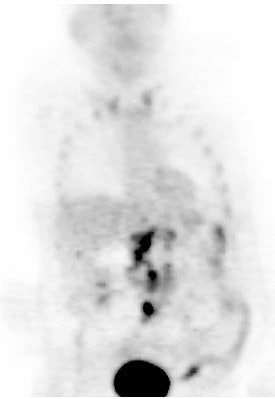
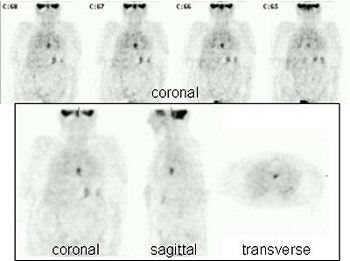 |
| FUO caused by the replacement of an aortic valve. Image courtesy of Dr. Stefan Dresel. |
The patient population consisted of 39 patients with FUO who were imagined on an Axis gamma camera with the company’s Gamma-PET AZ coincidence detection upgrade (Picker International, now Philips Medical Systems, Andover, MA) after the injection of 370 MBq of 18F-FDG. Images were acquired with 2-3 bed positions. The data was reconstructed iteratively and attention correction was performed uniformly.
In 27 out of 39 patients, the hybrid FDG-PET scans showed a pathological focus of increased glucose metabolism. In 13 out of 27 patients, the focus was found in areas where prosthetic material had been previously implanted, including in the hip joint and aortic valve. Six patients presented with pathological uptake in the lungs after being in intensive care, while eight others had lesions in the abdomen and abdominal organs and were found to be suffering from systemic inflammatory diseases.
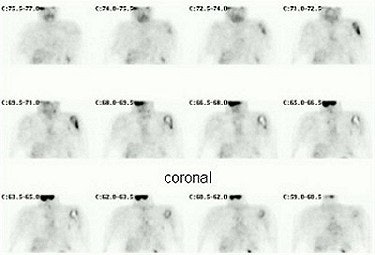 |
| In this case, a prosthesis in the left shoulder was the reason for FUO. Image courtesy of Dr. Stefan Dresel. |
"These lesions were not diagnosed by conventional methods and were confirmed by the success of therapy or the reimplantation of the prosthetic material," Dresel said.
The group concluded that hybrid FDG-PET delivered positive findings in 69% of the FUO patients and was superior to other modalities. Based on these promising results, Dresel’s department is currently shifting its diagnostic algorithm to perform FDG-PET early in the diagnostic workup of patients suffering from FUO, he wrote in an email to AuntMinnie.com.
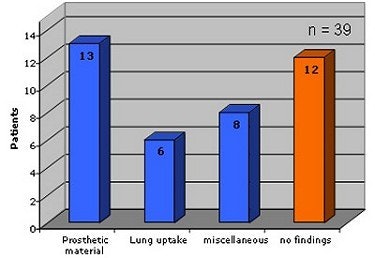 |
| This chart outlines the various causes of FUO in this study. Graphic courtesy of Dr. Stefan Dresel. |
"It still depends on the clinicians we are talking to in order to convince them (of the value of FDG-PET)," Dresel wrote. "But we only rarely perform granulocyte scintigraphy anymore, a method which was and is still widely used in these patients."
Scintigraphy for late-stage imaging
Scintigraphy using 111indium granulocytes has proven useful for imaging infection and chronic inflammatory bowel disease, but its results with FUO has been mixed, according to a group from the University of Copenhagen.
"The use of 111indium scintigraphy in FUO is special, because the test typically is used at a late stage when several other tests have been performed," wrote Dr. Andreas Kjaer, Ph.D., and Dr. Anne-Mette Lebech, Ph.D., in the Journal of Nuclear Medicine. "The high predictive value of negative scintigraphy findings may be especially valuable for ruling out an infectious cause of FUO" (JNM, February 2002, Vol. 43:2, pp.140-144).
This retrospective review was conducted over a six-year period on 31 cases with suspected FUO. Autologous granulocytes were labeled with 111In-tropolone and a dose of 9-12 MBq labeled granulocytes was injected intravenously, within one hour of labeling. Patients were imaged 20-24 hours after the injection of labeled granulocytes using a gamma camera with a medium-energy, general-purpose collimator (Millennium or XRT, GE Medical Systems, Waukesha, WI).
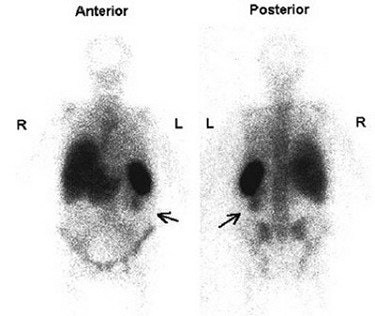 |
| True-positive scintigram shows left-sided pyelonephritis (arrows) as cause of FUO. Reprinted by permission of the Society of Nuclear Medicine from: Kjaer, A., et al. Diagnostic Value of 111-In-Granulocyte Scintigraphy in Patients with Fever of Unknown Origin. J Nucl Med 2002; 43:140-144. |
"The diagnostic value of 111In-granulocyte scintigraphy was evaluated by its ability to identify an infectious cause of FUO or chronic inflammatory bowel disease as the cause of FUO," the authors explained.
Out of 31 patients, a final diagnosis was obtained in 71% of the cases. In 26%, an infectious focus or chronic inflammatory bowel disease was the culprit. Scintigrams were considered true-positive in 75% of the cases and false-negative in 25%.
In 14 patients, noninfectious causes included neoplasms, Still’s disease, and cerebrally triggered fever. In nine patients, no cause was found and the majority recovered spontaneously. For these 23 patients, scintigrams were true negative in 83% cases and false-positive in 17%.
Overall, the sensitivity of 111In-granulocyte scintigraphy was 75%, the specificity was 83%, the positive predictive value (PPV) was 60%, and the negative predictive value (NPV) was 90%.
"Is this a high diagnostic performance?" the authors asked. "For many types of tests, performances in this range would make the test obsolete. For example, if the test was used for screening or as a first-line test." Instead, the authors advocated using scintigraphy when other tests have failed, bearing in mind that "negative scintigraphy findings have a high predictive value."
As a side note, the authors pointed out that a full 20% of their original patient population did not fulfill the Petersdorf criteria for FUO. "This fact underscores the importance of a careful definition of FUO and a careful review of cases when those cases are used to establish the diagnostic value of a test investigating FUO," they said.
FDG-PET for front-line testing
In a second SNM talk, Dr. Wim Oyen from the University Medical Center Nijmegen in the Netherlands shared his group’s results with FDG-PET as a way to guide further testing.
"Our hospital, being a tertiary referral hospital for patients with febrile diseases, has a little bit of a peculiar population. We have an unusually high percentage of patients without a diagnoses...57% of our patients are referred for second opinion," Oyen explained.
In this retrospective study, 35 patients underwent whole-body FDG-PET scans on an ECAT EXACT system (Siemens Medical Solutions, Erlangen, Germany). The median duration of fever before FDG-PET imaging was no less than two months, Oyen said.
FDG-PET images were reconstructed by an iterative method with segmented attenuation correction, and two staff members interpreted all FDG-PET scans. The results were compared to conventional diagnostic methods. Abnormal FDG-PET scans were considered useful if the uptake pointed to the location where the cause of the fever was eventually found.
According to the results, 23% of the patients were diagnosed with infection, 10% with malignancy, 3% with vasculitis, and 28% with other diseases, such as neoplasm, drug fever, and non-infectious inflammatory diseases. Fever remained unexplained in 36% of the cases.
"If we look at the overall results, 43% of all PET scans were abnormal. If abnormal, FDG-PET was considered helpful in the diagnosis in 87% of the cases," Oyen said. These results would make FDG-PET especially valuable if ordered early in the work-up of FUO because it would identify organs or tissue where the cause of fever is to be found, adding that the point of this exam is not final diagnosis but targeting the focal cause of disease.
 |
| A 65-year-old man presented with fever, weight loss, and diarrhea. Laboratory tests, chest x-ray, abdominal CT, and colonoscopy exams did not result in an explanation for his symptoms. This FDG-PET scan demonstrated increased FDG uptake in multiple cervical and abdominal lymph nodes. Biopsy confirmed a diagnosis of Hodgkin’s lymphoma. Image courtesy of Dr. Chantal Bleeker-Rovers. |
The group found that the PPV of FDG-PET in all 39 patients was 84% and the NPV was 90%. The other advantages of FDG-PET exams include high resolution, its strength in finding disease in the central skeleton, and its high reader concordance, Oyen said.
They concluded that FDG-PET is a worthwhile early imaging modality in FUO because it contributed to the eventual diagnosis in 41% of the patients whose previous test results had proved unsatisfactory.
"The earlier the diagnosis the better," he said. "You don’t have to make the final diagnosis with FDG-PET. You just have to guide the clinician and get the patient out of the hospital earlier."
In an e-mail to AuntMinnie.com, study co-author Dr. Chantal Bleeker-Rovers said that the group is working on a prospective study for a final validation of FDG-PET in FUO cases.
"In anticipation of the results of this prospective study, we now routinely use FDG-PET in cases of FUO when a history, physical examination, routine laboratory tests, blood cultures, serology, chest radiograph, and abdominal ultrasound do not result in a final diagnosis," she said. "When FDG-PET shows abnormal results, additional diagnostic tests such as biopsy, tissue cultures, or surgery are needed to define the exact cause of these abnormalities since FDG-PET cannot differentiate between infection, inflammation, or malignancy."
However, the group prefers using FDG-PET to other modalities, especially if there are no specific symptoms or abnormal lab results to provide guidance. "Multimodality imaging (except for chest x-ray and abdominal ultrasound) is only used to confirm the abnormalities found on FDG-PET or in patients with severe complaints and normal FDG-PET," she explained.
By Shalmali PalAuntMinnie.com staff writer
August 22, 2003
Related Reading
SARS presents distinct radiological patterns, May 6, 2003
Radiologists’ skills crucial in event of bioterrorist attack, March 14, 2003
MRI shows progression of West Nile virus encephalitis, December 5, 2002
CT spots sentinel pneumonia in 9-11 rescue worker, September 25, 2002
CT is the gold standard for inhalation anthrax imaging, November 29, 2001
Copyright © 2003 AuntMinnie.com




















