The SNM believes that a move by the Centers for Medicare and Medicaid Services (CMS) to bundle reimbursement for radiopharmaceuticals into payment for nuclear medicine procedures could result in reduced patient access for imaging studies.
CMS recently reclassified diagnostic radiopharmaceuticals as "supplies" rather than "drugs," the SNM said this week at its annual meeting in New Orleans. The change effectively bundles the radiopharmaceutical and procedure payments and results in reimbursement for radiopharmaceuticals that can be half the cost of producing the tracers, the Reston, VA, society said.
The SNM made four recommendations for changing the current regulatory structure:
- Radiopharmaceuticals should be treated as drugs rather than supplies.
- CMS should continue to reimburse for radiopharmaceuticals at charges reduced to cost in 2008, while working with nuclear pharmacies and vendors to develop a new standard payment methodology.
- All radiopharmaceuticals should qualify for the same bundling threshold ($60) in 2008 as other drugs.
- CMS should accept and use external data sources to identify and appropriately reimburse radiopharmaceuticals under the Hospital Outpatient Prospective Payment System, as the agency does for other drugs.
Related Reading
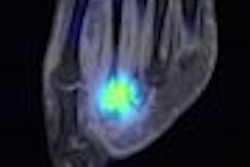
SNM's Images of the Year show molecular imaging's head-to-toe prowess, June 16, 2008
Nuclear medicine must overcome obstacles to flourish in the future, June 15, 2008
SNM explores feasibility of U.S. medical isotope source, May 22, 2008
Canadian government to stop development of Maple reactors, May 16, 2008
New U.S. budget funds nuclear medicine programs, January 14, 2008
Copyright © 2008 AuntMinnie.com