A clinical examination is as accurate as MRI for the diagnosis of meniscal tears and an anterior cruciate ligament (ACL) rupture, researchers reported Saturday at the 2002 meeting of the American Academy of Orthopedic Surgeons this month in New Orleans.
Dr. Yavuz Kocabey and associates at the University of Kentucky in Lexington evaluated 50 consecutive patients with 65 defined pathologies of medial/lateral menisci and ACL who presented to the university’s orthopedics division during a recent six-month period.
"While MRI has become the gold standard for accurate, noninvasive evaluation of internal pathologies of the knee, its high cost precludes its routine use as a diagnostic tool," Kocabey said.
The study was undertaken to determine whether MRI yields superior results to a clinical examination. Pathologies such as plica, chondral fractures, and loose bodies -- which can mimic meniscal tears and lead to false-positive MRI results -- were excluded from the analysis.
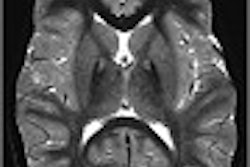
After the clinical examination, the same orthopedic surgeon evaluated the MRI findings in patients prior to arthroscopy. The MRI scans in this trial were performed at four different centers using three 1.5-tesla scanners and one 1-tesla scanner.
The surgeon performed each arthroscopic procedure by extensively probing all structures, and photographs of all cases were taken to confirm arthroscopic findings. Arthroscopy was considered to be the diagnostic standard, and the results were evaluated and based on arthroscopic findings and diagnosis.
Results of the clinical diagnosis of medial and meniscal tears were equal (80% and 92% accuracy, p > 0.05) to MRI results (80% and 90% accuracy, p > 0.05).
Clinical examination was accurate in diagnosing ACL lesions in 100% of cases, while MRI was accurate in 98% (p > 0.05).
As for limitations, Kocabey cautioned that the analysis focused on the experience of a single surgeon.
"Using a single surgeon’s experience in our study may introduce potential bias because the results are thus dependent on that particular surgeon’s skills and knowledge," he said. "We know that a different surgeon might have achieved different results for this set of patients."
Based on the findings, Kocabey said that MRI is not generally needed to confirm the surgeon’s diagnosis provided that the diagnosis is based on a comprehensive clinical examination and patient history.
MRI's accuracy might improve as radiologists gain more experience and use more effective protocols, he said, and the widespread use of larger magnets could also help. But at the present time, MRI does not offer an advantage over clinical examination alone for the routine use in the diagnosis of meniscus and ACL pathology, Kocabey concluded.
Still, other researchers have reached different conclusions. Investigators with the Dutch Knee Project in Leiden reported that MRI triage for arthroscopy was a worthwhile method for evaluating patients with sub-acute knee pain. In this prospective, randomized multicenter trial, 430 patients underwent MR imaging on a 0.5-tesla Gyroscan (Philips Medical Systems, Best, the Netherlands). The group calculated the sensitivity and specificity of MRI in all of the patients, including those who underwent arthroscopy.
Out of 430 patients, 209 with negative MR imaging results were randomized for arthroscopic (105 patients) or for conservative treatment (104 patients). Of the 105 patients randomized for arthroscopy, 93 actually underwent the procedure.
Arthroscopic treatment was necessary in 13 of 93 patients with a negative diagnosis at MR imaging. Arthroscopic treatment was necessary in 179 of 200 patients with a positive MR diagnosis, for a sensitivity of 93.2% and a specificity of 79.2%. Sensitivity and specificity corrected for randomization were 87.3% and 88.4%.
Sensitivity and specificity corrected for randomization, respectively, were 84.1% and 94.2% for the diagnosis of medial meniscal tears and 69.5% and 94.5% for the diagnosis of lateral meniscal tears at MR (Radiology, June 2002, Vol. 223:3, pp.739-746).
The group updated its results at the 2002 RSNA meeting. They found MRI triage for knee injuries to be cost-effective. The total cost of triage with MRI was 2,581 euros ($2,797 U.S.) versus 2,770 euros ($3,002 U.S) for arthroscopy without MRI triage.
By Jill SteinAuntMinnie.com contributing writer
February 11, 2003
Related Reading
MRI pinpoints meniscal tears, proves less valuable for knee trauma, January 9, 2003
Turf Wars in Radiology, Part V: Radiologists, orthopedists put best foot forward, October 1, 2002
Scenes from the Polyclinic: a case study, February 19, 2002
Olympic skiers tear up slopes -- and knees, February 18, 2002
Copyright © 2003 AuntMinnie.com