
Endoanal MRI and endoanal ultrasound demonstrate nearly equal capabilities for depicting external anal sphincter (EAS) defects in patients with fecal incontinence, although they have slight differences in positive predictive value and sensitivity. A four-year, 13-center prospective study conducted in the Netherlands has found that both modalities are sensitive tools for preoperative assessment and both techniques can be used to depict surgically repairable anterior EAS defects.
"There is no significant difference between endoanal MR imaging and endoanal ultrasound in the depiction of external anal sphincter defects," the authors wrote in Radiology. The authors, led by Annette Dobben, Ph.D., are from the Academic Medical Center and Onze Lieve Vrouwe Gasthuis, both in Amsterdam, as well as the University Hospital Maastricht in Maastricht, the Netherlands (February 2007, Vol. 242:2, pp. 463-471).
The study cohort consisted of 214 women and 23 men with fecal incontinence who were examined with endoanal MRI or ultrasound between December 2001 and May 2005.
"All eligible patients were referred for standardized specialized pelvic floor rehabilitation after standardized diagnostic workup, including imaging," the authors wrote. "If pelvic floor rehabilitation failed, overlapping anterior anal sphincter repair was considered as the next available treatment option for patients with an EAS defect."
All patients in the study had both endoanal ultrasound and MR performed. The endoanal ultrasound was performed by six clinicians and one sonographer, each of whom had 10 or more years of experience, prior to endoanal MR. The ultrasound studies were conducted with either a Brüel & Kjaer model 3535 (Nærum, Denmark) or and Aloka Multiview (Tokyo) system with a radial endoscopic probe and a sonolucent plastic cone.
All endoanal MR exams were performed by technologists with between one and five years of experience. The MR studies were conducted on either a 1-tesla Philips Medical Systems Gyroscan ACS-NT (Andover, MA) or a 1.5-tesla GE Healthcare Horizon EchoSpeed (Chalfont St. Giles, U.K.) system with a 19-mm diameter dedicated endoanal coil. All patients fasted for four hours prior to the MR studies to reduce artifacts from bowel peristalsis, the authors noted.
The endoanal ultrasound images were reviewed by one of six observers from the seven centers where the exams were conducted, while the endoanal MR images were reviewed by one of three observers -- each of whom was a radiologist with eight to 12 years of experience in evaluating abdominal MR images, according to the researchers.
"Both endoanal ultrasound and endoanal MR images were evaluated separately," they reported. "Observers were blinded to the findings of the other technique and to the medical history of the patients, except for age, sex, and the presence of fecal incontinence."
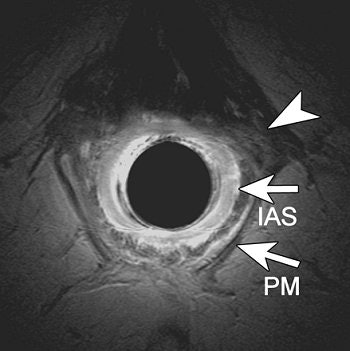 |
| A transverse endoanal T2- weighted fast spin-echo (2500/70) MR image (a) obtained at proximal anal canal in 69-year-old woman with complicated vaginal delivery who had undergone hysterectomy. Anal sphincters were classified as intact. Retrospectively, slight asymmetry of structures (arrowhead) located left anterolateral to the internal anal sphincter (as compared with the right anterolateral site) can be seen; these most likely represent the EAS defect diagnosed at surgery. |
A total of 168 of the 237 patients (71%) had an EAS defect visible on either endoanal ultrasound or MRI. The researchers found that an EAS defect was depicted on endoanal MRI in 31 patients, for 60 patients on endoanal ultrasound images, and 77 patients had an EAS defect visible in both modalities. They noted that the patient group with EAS defects visible only on ultrasound was older than the group whose defects were visible on both modalities.
Thirty-six of these patients with EAS defects depicted on imaging (21%) underwent anterior anal repair approximately 10 months after their exams. Of this group, 31 of 36 anterior EAS defects were detected in surgery (86%), while no defects could be found in five of the patients (14%).
"There was no significant difference in the depiction of EAS defects between endoanal MR imaging and endoanal ultrasound," the researchers wrote.
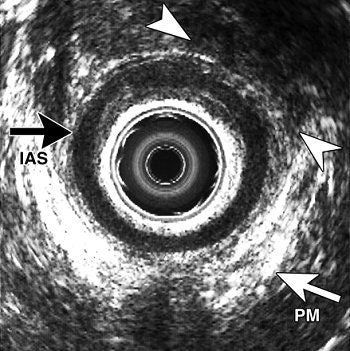 |
| A transverse endoanal US image (b) obtained in same patient shows EAS defect at upper edge (arrowheads) in proximal anal canal. This finding was confirmed during anal sphincter repair, which revealed an anterior EAS defect. Top of the figure is anterior. IAS = internal anal sphincter; PM = lower edge of puborectal muscle. Figure 3a,b. Dobben AC, Terra MP, Slors JFM, et al. "External anal sphincter defects in patients with fecal incontinence: comparison of endoanal MR imaging and endoanal US." Radiology 2007; 242: 463-471. |
The scientists reported that the sensitivity for detecting EAS defects was 81% for endoanal MRI and 90% for endoanal ultrasound. The positive predictive value for detecting EAS defects was 89% for endoanal MRI and 85% for endoanal ultrasound, while complete agreement between both techniques was 69%. They noted that specificity and negative predictive values were low or could not be calculated in their patient cohort.
The researchers observed that a major limitation of the work was partial verification bias, because they did not know the surgical findings of the patient group that did not have surgery during the study duration. They stated that this may have led to an overestimation of sensitivity and an underestimation of specificity. In addition, they wrote that only endoluminal imaging of EAS lesions was evaluated and they did not include anal sphincter findings in their comparative study.
Although the team was able to validate its findings only in the 36-patient subgroup that underwent surgery, the scientists believe that the fair agreement between the modalities in the larger cohort of patients demonstrates that endoanal MRI and ultrasound are sensitive tools for depicting surgically repairable anterior EAS defects.
"When we validated our results in a small cohort of patients and compared these results with surgical findings, we concluded that both imaging techniques can be considered useful in the selection of patients for surgery," they wrote.
By Jonathan S. Batchelor
AuntMinnie.com staff writer
February 7, 2007
Related Reading
Endoanal ultrasound improves diagnosis of childbirth-related anal sphincter tears, July 11, 2005
Ultrasound expands role in incontinence, bladder tumors, August 11, 2005
US combo boosts detection, characterization of perianal inflammation, January 15, 2004
Endoscope guides precise Botox delivery for anal fissure treatment, June 18, 2003
Radiofrequency therapy shows promise as treatment for fecal incontinence, June 11, 2002
Copyright © 2007 AuntMinnie.com




















