MRI and CT allow clinicians to obtain sensitive 3D images of the spine, intervertebral disks, and neural structures. However, both modalities are limited in their ability to provide a dynamic stress study of the axial skeleton because of patient positioning. More specifically, normal compressive loads on the spine are decreased in conventional imaging studies because of the recumbent patient positioning.
Upright MRI units have been shown to provide dynamic stress and coupled motions studies of the spine, but may be limited by cost as well as poor-quality images as a result of motion artifacts and magnet strength.
 |
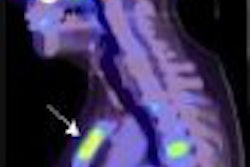
| Above, midsagittal T2-weighted MRI showed increase in stenosis at the L4 level by 2.0 mm with ventral thecal sac compression with axial loading (below). All images courtesy of Dr. Gerald Anzalone. |
 |
Moreover, a number of studies have suggested that conventional MRI and CT are at considerable risk for failing to detect essential narrowing of the spinal canal when only the recumbent patient scanning position is utilized. This has been shown in patients with lumbar spinal pain combined with sciatica, radiculopathy, neurogenic claudication, or suspected lumbar spinal stenosis, according to research conducted by Dr. Jan Willen, Ph.D.; Dr. Barbro Danielson, Ph.D.; and colleagues at Sahlgrenska University Hospitals in Goteborg and Molndal, Sweden (Spine, December 1, 2001, Vol. 26:23, pp. 2607-2614; Acta Radiologica, November 1998, Vol. 39, 6, pp. 604-611; Spine, December 15, 1997, Vol. 22:24, pp. 2968-2976).
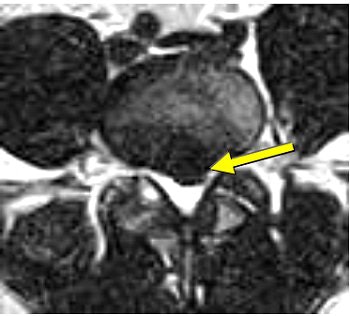 |
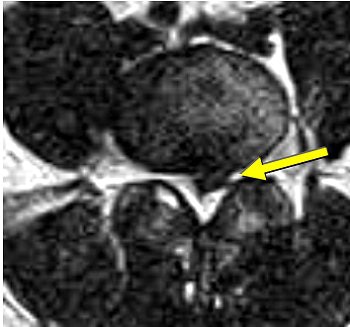
| Same patient as above. Top, transaxial T2-weighted image showed left L4 spinal nerve root compromise with axial loading (below). |
 |
Although no CPT code is currently available for axial-loaded imaging, this technique offers increased diagnostic specificity for dynamic lumbar stenosis and enhanced visualization of dynamic spinal responses to compressive axial forces (versus static pathoanatomical evaluation).
Axial-loaded advantage
Willen and Danielson have also shown that axial-loaded imaging, during recumbent MRI or CT, simulates weight-bearing forces in the lumbar spine, provoking narrowing of the central spinal canal and neural foramina, and increasing the diagnostic accuracy of dynamic spinal stenosis. Dynamic stenosis has been defined in literature as a change in the cross-sectional dural sac area of greater than 15 mm² resulting in a decrease in the dural sac area to less than 75 mm (Spine, December 1, 2001, Vol. 26:23, pp. 2607-2614; Acta Radiologica, November 1998, Vol. 39, 6, pp. 604-611; Spine, December 1, 2001, Vol. 26:23, pp. 2601-2606).
Willen and Danielson's group found that 79% of patients with combined low back and leg symptoms experienced a significant reduction of the dural sac cross-sectional area during axial compression; 35% of patients passed the borderlines for relative stenosis (100 mm²) or absolute stenosis (75 mm²); 36% of patients experienced deformation of the dural sac during axial compression; and 13% of patients experienced a narrowing of the lateral recess during axial compression (Spine, December 15, 1997, Vol. 22:24, pp. 2968-2976).
 |
| Increased conspicuity of L4-L5 disk bulge and 2.0 mm increase in stenosis at the L4-L5 level with axial loading. |
 |
Willen and Danielson studied patients with suspected clinical lumbar spine encroachment, and found a significant decrease in the dural cross-sectional area in 80% of the patients undergoing axial-loaded CT and 76% of the patients who underwent axial-loaded MRI (Spine, December 1, 2001, Vol. 26:23, pp. 2601-2606).
Axial loading may show functional spinal changes in apparently normal segments. Dr. Shinji Kimura, Ph.D, and colleagues found that the axial force of 50% body weight in supine posture simulates the upright lumbar spine morphologically, significantly decreasing the disk height at L4-L5 during compression (Spine, December 1, 2001, Vol. 26:23, pp. 2596-2600).
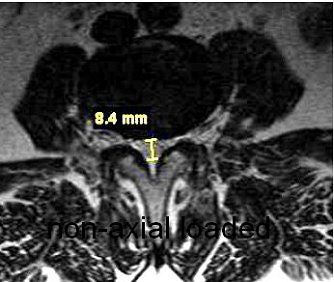 |
| Nonaxial loaded (above), transaxial T1-weighted images showed increased stenosis by 3.2 mm of the central spinal canal at the L3-L4 level with axial loading (below). |
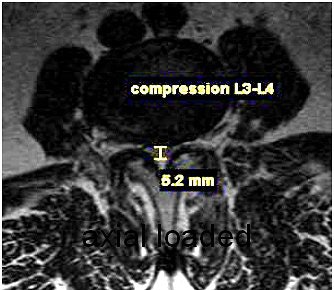 |
A survey of patients from a private practice setting who underwent axial-loaded imaging demonstrated an increase in the conspicuity of focal disk bulging and herniation, as well as an increase an anterolisthesis or retrolisthesis ("Axial loaded magnetic resonance imaging of the lumbar spine in a chiropractic patient population," Proceedings of the 2006 Conference on Chiropractic Research, Chicago).
Dr. Akio Hiwatashi's group found that axial loading during MR imaging of the lumbar spine can influence treatment decisions for symptomatic spinal stenosis from conservative management to decompressive surgery based on the findings obtained from axial-loaded MR images (American Journal of Neuroradiology, February 2004, Vol. 25:2, pp. 170-174).
 |
| Above, nonaxial loaded CT scan of postsurgical lumbar fusion patient showing increased stenosis of the thecal sac at the L3-L4 level with axial loading (below). |
 |
 |
| A Portal Gravity System axial-loading device, which is compatible with commercially available standard MRI and CT systems, simulates the upright position of the spine during recumbent imaging. |
The Sahlgren group also found that axial loading on supine MRI produces coronal Cobb angles similar to standing radiographs, providing a way to acquire reliable Cobb angles without radiation in the monitoring of idiopathic scoliosis (Spine, December 15, 2006, Vol. 31:26, pp. 3039-3044).
Reported contraindications to axial-loaded lumbar spinal imaging include severe osteoporosis, fracture, or skeletal malignancy. Researchers recommend that osteoporotic patients with suspected lumbar spinal canal stenosis undergo a conventional or preaxial-loaded MRI scan prior to undergoing spinal loading to determine if the introduction of an axial load is appropriate (Spine, December 1, 2001, Vol. 26:23, pp. 2607-2614).
The results from axial-loaded MRI or CT may influence management for patients with low back pain combined with sciatica, radiculopathy, or neurogenic claudication, or in those with suspected lumbar spinal stenosis, and axial-loaded imaging should be considered a viable imaging alternative in selected patients.
By Dr. Gerald A. Anzalone, D.C.
AuntMinnie.com contributing writer
May 29, 2007
Dr. Gerald Anzalone is a 1997 graduate of New York Chiropractic College in Seneca Falls, NY. He is a consultant for Portal Medical of Logan, UT. Anzalone is a member of the Foundation for Chiropractic Education and Research and the American Public Health Association. He practices in Peekskill, NY.
Related Reading
Disk transplantation shows promise as treatment for spine disease, March 23, 2007
PACS results in more incidental cervical spine MR findings, November 29, 2006
MR study shows how whiplash can be perpetual pain in the neck, November 16, 2006
Chiropractic imaging under Medicare attracts attention, August 23, 2005
Copyright © 2007 AuntMinnie.com