The spectrum of abnormalities detected at MRI in women with stress urinary incontinence can be classified into two categories: findings related to urethral sphincter deficiency (ISD) as well as defects of the urethral support ligaments, and/or urethral hypermobility (UH).
These abnormalities may include a small urethral sphincter, funneling at the bladder neck, asymmetric pubococcygeus muscle, abnormal vagina shape, and an increased vesicourethral angle (RadioGraphics, July-August 2006, Vol. 26:4, pp. 1135-1149).
In a study released last year, Dr. Katarzyna Macura, Ph.D., and colleagues from the Johns Hopkins Medical Institutions in Baltimore demonstrated the feasibility of intraurethral MRI for the in vivo assessment of the female urethra. They also used an endourethral MR coil to determine the anatomy of the urethra and periurethral attachments.
They found that this technique offered detailed visualization, and measurements, of the muscular layers of the urethral sphincter and permitted the evaluation of supporting ligaments (Journal of Magnetic Resonance Imaging, July 2004, Vol. 20:1, pp. 153-159).
Now the group has taken its research a step further in a study that assessed if MR findings could predict whether a patient had ISD or UH, and whether those results correlated with urodynamics.
 |
| Visualization of the laxity of the right periurethral ligament (arrow) on endovaginal MRI in a woman with UH. Image courtesy of Dr. Katarzyna J. Macura, Ph.D., Johns Hopkins University. |
"SUI is defined as the involuntary urine leakage during increasing intra-abdominal pressure such as during cough, strain, or even during exercise. This is the most common time of urinary incontinence in women. It is a significant health and social problem and quite expensive to manage," Macura said in a talk at the 2007 International Society for Magnetic Resonance in Medicine (ISMRM) meeting in Berlin.
For this pilot study, 18 patients with stress urinary incontinence were enrolled. The 1.5-tesla MR (Signa Excite, GE Healthcare, Chalfont St. Giles, U.K.) protocol included endocavitary and standard pelvic imaging. MR techniques for T2-weighted fast spin echo in three planes were intraurethral, endovaginal or endorectal, and pelvic MRI with pelvic phased-array coil, and dynamic strain imaging.
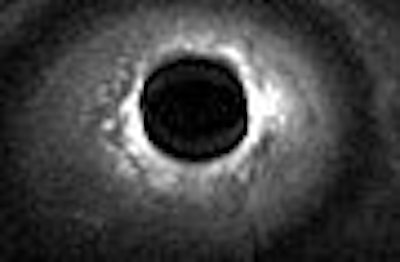
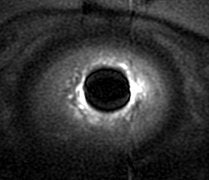 |
| Intraurethral MR shows details of urethra sphincter muscles (outer T2 dark striated muscle and inner T2 bright smooth muscle). Image courtesy of Dr. Katarzyna J. Macura, Ph.D., Johns Hopkins University. |
ISMRM session moderator Dr. Kaori Tagashi asked Macura about the timing of this imaging protocol. Macura said that the above protocol was for research purposes and the entire exam took 40 minutes. In a clinical setting, the protocol would be streamlined to 20 minutes with just endovaginal and strain imaging.
Patients were categorized as UH, ISD, or mixed. MR criteria for UH included a urethral mobility angle of greater than 30° and abnormal bladder neck descent. For ISD, the criteria included sphincter length above pubis (less than 3 cm) and sphincter defect or thinning. MR findings were correlated with multiple urodynamic parameters such as Valsalva leak point pressure (VLPP), maximum urethral closure pressure (MUCP), and Q-tip test for urethral mobility.
According to the results, "among 12 patients, MRI showed a sensitivity of 92% (for) predicting UH," Macura said. "One patient, who had no MRI findings of urinary incontinence, actually had a UH diagnosis on urodynamics. Specificity was very high (100%). All patients with UH showed at least partial or complete disruption of the periurethral ligament and 10 patients showed widening of vagio-levator attachments."
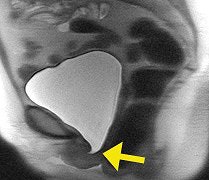 |
| Strain imaging steady-state fast spin echo (SSFSE) of urethra mobility and bladder neck competence assessment. Note hypermobility of urethra that assumed horizontal position and bladder neck funneling (arrow). Image courtesy of Dr. Katarzyna J. Macura, Ph.D., Johns Hopkins University. |
With ISD, MRI predicted four cases with 100% sensitivity and specificity, Macura said. Specific findings included shortening in the urethra and bladder neck funneling. Two cases of mixed incontinence were diagnosed with 100% accuracy, she added. Finally, the researchers found a high correlation between VLPP and sphincter muscle length, Q-tip mobility, and hypermobility angle on MRI, and between MUCP and posterior striated muscle thickness of the midurethra.
"MRI has the potential to become central not only to understanding the cause of stress urinary incontinence, but also (contributes) findings that are predictive of UH and ISD," she said. "Also MRI findings correlate well with urodynamics and can support the classification of patients into the two categories, which may require differentiate treatment modalities for these patients."
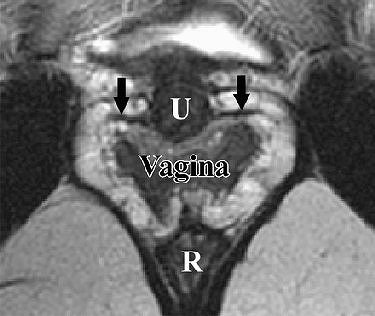 |
| Pelvic MR images of a continent 32-year-old woman. Imaging parameters were as follows: 3800/99, 6.0-mm section thickness, 2.0-mm section spacing, four signals acquired, 20 x 20-cm field-of-view. R = rectum. Above, axial T2-weighted fast spin-echo image obtained at the level of the upper urethra shows the paraurethral ligament (arrows) extending from the lateral wall of the urethra (U). Below, axial image obtained at the level of the midurethra shows the periurethral ligament (arrows) extending between the medial aspects of the pubococcygeus muscle (arrowheads) and coursing ventrally to the urethra (U). |
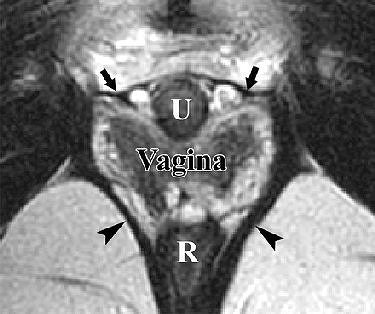 |
| Figures 3a,b. Macura KJ, Genadry RR, Bluemke DA, "MR imaging of the female urethra and supporting ligaments in assessment of urinary incontinence: Spectrum of abnormalities." RadioGraphics 2006; 26:1135-1149. |
ISMRM session moderator Dr. Nandita D'Souza asked Macura if there will be some distortion and reduced prolapse when endocavitary coils are inserted into the pelvic floor. Macura said that the coils were used for anatomic imaging and then removed for strain imaging so that the pelvic floor could relax.
"For each part of the exam, we have a purpose," Macura explained. "So when we look at the sphincter, we only focus on the quality of the muscle for which the intraurethral coil provides good detail. When we look at the vagio-levator attachments, then we may decide to use either an endorectal probe versus an endovaginal probe." In an e-mail interview with AuntMinnie.com, Macura clarified that endocavitary coils are not used when the pelvic floor is evaluated dynamically.
With regard to bladder filling, Macura said the protocol was to start with an empty bladder and perform the most invasive imaging. By the end of that exam, the bladder was full and strain imaging could be done.
For the time being, MRI should serve as an adjunct imaging technique to urodynamics, and that referring physicians do find the MR results helpful, Macura told AuntMinnie.com. The urogenital and gynecological specialists that she works with ask that she obtain as "much information as possible when dealing with complex situations and recurrences before deciding on any course of action, particularly surgical," Macura stated.
Whether MRI could replace urodynamics remains to be seen. One major issue that needs to be looked at is the cost-effectiveness of MR in this setting. Macura's group recently published an updated article on the pathophysiology of female urinary incontinence and MR in Abdominal Imaging (July 3, 2007).
"MRI could replace urodynamics when intravesical and abdominal pressures can be obtained at the same setting as getting the MR images. This would be the next step in investigating whether MRI can replace urodynamics if such catheters were available. More studies are otherwise needed to assess the role of MR in assessing bladder and urethral functions," Macura stated. "Ultrasound could compete with MR as a cost-effective, initial means of evaluation. Both techniques need to be evaluated in the same clinical setting."
By Shalmali Pal
AuntMinnie.com staff writer
July 27, 2007
Related Reading
External anal sphincter defect findings nearly equivalent on MR, US, February 7, 2007
Total hysterectomy not associated with urinary incontinence, November 23, 2006
Copyright © 2007 AuntMinnie.com




















