A solitary pulmonary nodule is easy to define -- a roundish lesion smaller than 3 cm in diameter that is surrounded by pulmonary parenchyma and no other pulmonary abnormalities. Tracking these small lesions is another matter. Different modalities have their strengths and weaknesses in lung cancer imaging. Obviously, CT is a major weapon in the thoracic imaging arsenal with FDG-PET, sonography, and angiography acting as supplements.
MRI has also contributed to a greater understanding of small nodules, particularly with the introduction of more advanced protocols. Two studies in the American Journal of Roentgenology suggest that dynamic MRI and 3-tesla MRI, respectively, can depict clinically significant small nodules, but also distinguish between benign and malignant lesions. In a related paper, Japanese nuclear medicine specialists look at the value of MR for assessing cerebral lesions from metastatic lung cancer.
Depicting small tumors
Historically, thoracic CT is the gold standard for assessing the intrathoracic spread of non-small cell lung cancer (NSCLC) with MRI turning in a less desirable performance as the modality suffers from low signal-to-noise ratio (SNR) and susceptibility artifacts. But more sophisticated MR techniques, including turbo spin echo (TSE), short tau inversion recovery (STIR), and half-Fourier acquisition single-shot turbo spin echo (HASTE), on higher field strength magnets could render it a more suitable test.
For this study, Dr. Chin Yi and colleagues looked at 122 patients with pathologically proven NSCLC and no suspected metastatic lesions. Adenocarcinoma was the lung cancer subtype in 47% of the subjects. Contrast-enhanced chest CT (LightSpeed QX/i, LightSpeed Ultra, or Ultra16, GE Healthcare, Chalfont St. Giles, U.K.) was done about five days before the MRI.
Yi and co-authors are from the Samsung Medical Center, Sungkyunkwan University School of Medicine, Asan Medical Center, and University of Ulsan College of Medicine, all in Seoul, South Korea.
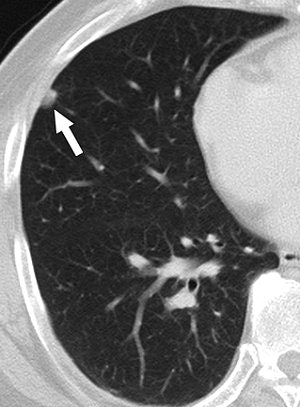 |
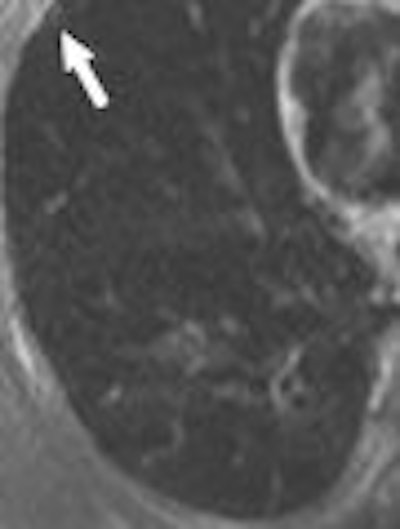
| A 58-year-old man with squamous cell carcinoma in right upper lobe and biopsy-proven anthracofibrotic nodule in lobe not containing primary tumor. Transverse lung-window CT scan at level of basal segmental bronchus shows 9-mm subpleural nodule (arrow) in right middle lobe. Nodule was pathologically proven anthracofibrotic nodule. |
All MR studies were done on a 3-tesla scanner (Achieva, Philips Medical Systems, Andover, MA). Sequences included breath-hold T2-weighted triple inversion black blood TSE with cardiac gating and T1-weighted 3D multishot turbo field echo during breath-hold. Two chest radiologists read the CT scans first, then the MR images, and then reviewed CT and MRI datasets simultaneously.
According to the results, "on both T1-weighted 3D turbo field-echo and T2-weighted triple inversion black blood TSE images, primary malignant cancer was well visualized in terms of margin characteristics, presence of satellite nodules, and cavitation," the authors wrote, adding that there were different MR detection rates for differently sized nodules (AJR, August 2007, Vol. 189:2, pp. 386-392).
 |
| Same patient as above. T1-weighted 3D turbo field-echo (B) and T2-weighted triple inversion black blood turbo spin-echo (C) images show 9-mm nodule (arrow) in right middle lobe. Nodule is subtle in C and not easily visualized. |
 |
| Yi CA, Jeon TY, Lee KS, Lee JH, Seo JB, Kim YK, Chung MJ, "3-T MRI: Usefulness for Evaluating Primary Lung Cancer and Small Nodules in Lobes Not Containing Primary Tumors" (AJR 2007; 189:386-392). |
More specifically, the primary nodule diameter on T2-weighted MR was 38.1 mm versus 38.4 on turbo field-echo MR and 38.7 on CT. On CT, the majority of nodules were spiculated or lobulated (97%). MR also accurately depicted 97% of these same morphological features.
The overall detection rate for small nodules in lobes that did not contain primary tumors was 57% for T1-weighted MRI and 56% for T2-weighted TSE imaging. The detection rate of noncalcified nodules on T1-weighted imaging was 53% and 57% for T2-weighted TSE MRI. Finally, the detection rates were 92% for both MR techniques for noncalcified lesions between 5 mm and 10 mm in diameter.
"Size comparison between T1-weighted 3D turbo field-echo and T2-weighted triple inversion black blood TSE sequences may help characterize small pulmonary nodules in lobes not containing primary tumors," the authors concluded.
Separating malignant from benign
Yi's results dovetailed with an earlier study out of Japan and Canada that found dynamic contrast-enhanced MRI could be used to decipher between benign and malignant nodules, based on MR enhancement characteristics.
Dr. Rei Kono's team retrospectively reviewed the records of 202 patients with single pulmonary nodules (based on CT exam) than ranged from 1 cm to 2.9 cm in diameter. Of these 202 cases, 144 were primary NSCLC and 31 were focal organizing pneumonia.
"Focal organizing pneumonia is difficult to differentiate from lung cancer. Our results indicate that lung cancer has a significantly lower maximum enhancement ratio and slope than focal organizing pneumonia," wrote Kono, who is from the department of radiology at Kurume University School of Medicine in Fukuoka, Japan. Study co-authors are from the university's departments of pathology and surgery, as well as from the University of British Columbia in Vancouver (AJR, January 2007, Vol. 188:1, pp. 26-36).
The subjects underwent scanning on a 0.5-tesla system (Magnex 50HP, Shimadzu, Kyoto, Japan) and the sequences included T2-weighted spin-echo and oblique sagittal or transverse imaging, all during breathhold. After the first spin-echo sequences, gadopentetate dimeglumine (Magnevist, Berlex Imaging, Wayne, NJ) was administered and contrast-enhanced dynamic MRI images were obtained from one to eight minutes. Images were analyzed for maximum enhancement ratio, time at maximum enhancement ratio, slope of time enhancement ratio curves, and washout ratio.
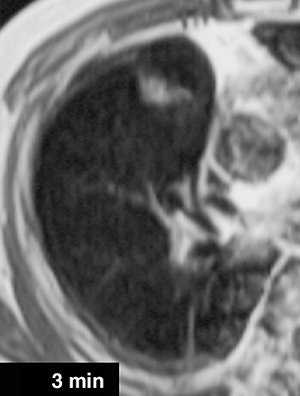
 |
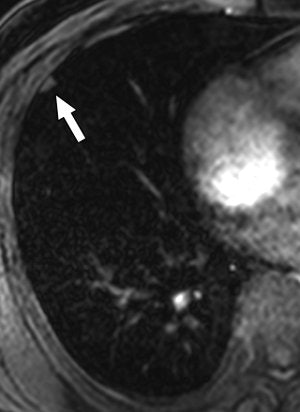
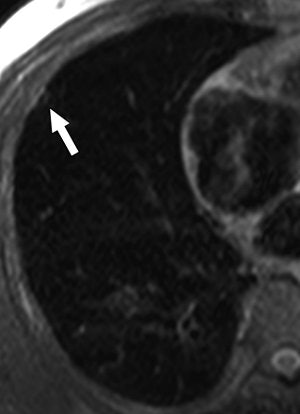
| A 68-year-old woman with focal organizing pneumonia in right middle lobe of lung. Above, dynamic MR image before IV injection of gadopentetate dimeglumine. Below, dynamic MR image obtained three minutes after IV injection of gadopentetate dimeglumine shows slightly heterogeneous enhancement that is strongest in early phase (three minutes = time at maximum enhancement ratio). Signal intensity before and three and six minutes (time at maximum enhancement ratio plus three) after contrast injection was calculated by each region of interest. Maximum enhancement ratio, 126%; slope, 42%/min; washout ratio, 15%. |
 |
| Kono R, Fujimoto K, Terasaki H, Müller NL, Kato S, Sadohara J, Hayabuchi N, Takamori S, "Dynamic MRI of Solitary Pulmonary Nodules: Comparison of Enhancement Patterns of Malignant and Benign Small Peripheral Lung Lesions" (AJR 2007; 188:26-36). |
According to the results, in 85% of 144 primary lung cancers, the time at maximum enhancement ratio was four minutes or less. In comparison, for benign lesions, the time was greater than four minutes. Lung cancers also had different maximum enhancement ratios and slopes than benign lesions. Using a maximum enhancement ratio of 100% or lower, the positive predictive value for malignancy was 92%. The sensitivity was 63% and the specificity was 74%.
The authors acknowledged that the sensitivity was relatively low and that "overlap of enhancement characteristics of dynamic MRI between focal organizing pneumonia and lung cancer is not surprising because malignant neoplasms and tissues with acute inflammatory lesions ... have increased blood flow, perfusion, and capillary permeability." But they noted that the slope was still steeper for focal organizing pneumonia than it was for lung cancer.
Cerebral metastases
MRI is commonly seen as the optimal screening tool to detect intracranial masses, including metastases from lung cancer. The strength of MR imaging in this setting is to delineate tumor margins and the extent of lesions. But the modality falls short in discriminating between benign and malignant cerebral lesions, which can impact patient management, according to Dr. Tamotsu Kita and colleagues from the National Defense Medical College in Tokorozawa, Japan.
Kita's group proposed adding thallium-201 (TI-201) SPECT to the imaging protocol to obtain more diagnostic information. For this study, 13 patients with intracranial masses were recruited. On their MRI exams, all showed ring-line enhancement. Two patients had cerebral metastases from lung cancer. The mean cerebral mass size was 3.1 cm.
Contrast-enhanced MRI was done a 1.5-tesla scanner (Signa Advantage, GE Healthcare) and axial T1- and T2-weighted images were obtained. For SPECT imaging, the subjects received 111 MBq of TI-201 chloride and scanning was done two hours later on a three-headed camera (GCA-9300A/HG, Toshiba, Tokyo).
Both sets of images were read by radiologists, nuclear medicine specialists, and neurosurgeons who rated the images on a five-point scale. "The 10 readers agreed that a focus that exhibited increased TI-201 uptake was a malignant lesion with vascularity ... whereas a focus that exhibited little or no TI-201 uptake was a benign lesion," the authors explained (Annals of Nuclear Medicine, July 2007, Vol. 21:5, pp. 251-256).
The sensitivity, specificity, and accuracy of the readers' diagnostic performance were evaluated and a ROC analysis was performed with the area under the ROC curves (Az) calculated for MR alone and MRI plus TI-201 SPECT.
According to the results, the average sensitivity for all 10 readers improved from 67% to 91% when SPECT was added to MRI. The average specificity for the group also increased from 67% to 100%. The readers' average accuracy jumped from 67% to 93% while the false-positive rate fell from 32% to zero. The false-negative rate dropped from 32% to less than 1%. The Az values for MR image readings for all 10 physicians was 0.730. This average was boosted to 0.971 for the combination of MR and SPECT.
"Correlative reading of TI-201 brain SPECT with contrast MR imaging seems to be an accurate method for discriminating between benign and malignant cerebral disease," the authors stated. "Our study showed that TI-201 brain SPECT imaging had an impact on interpretation performance in patients with ring-like enhanced lesions (on MR)."
They acknowledged that the small patient population, as well as the larger lesion size (smaller lesions would most likely have lowered diagnostic confidence to some degree) were two study limitations. However, they pointed out that based on inconclusive MR results, patients may undergo unnecessary craniotomies or stereotactic biopsies, both of which exceed the cost of a TI-201 SPECT scan. On the other hand, TI-201 SPECT may not be sensitive enough on its own and MR does offer a prompt diagnosis, they stated.
Future studies will have to broaden the scope of this research, including MRI/SPECT fusion as well as TI-201 SPECT paired with FLAIR MR, diffusion-weighted imaging, and perfusion-weighted imaging.
By Shalmali Pal
AuntMinnie.com staff writer
August 3, 2007
Related Reading
FDG uptake correlates with survival, biomarkers in NSCLC, June 19, 2007
Preventive brain radiation prolongs survival in advanced lung cancer, June 4, 2007
Copyright © 2007 AuntMinnie.com


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)





.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











