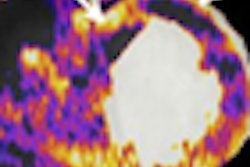
Breast MRI accurately reflects the pathologic extent of residual disease following neoadjuvant chemotherapy, and tumor size and contrast kinetics measured by MRI may be useful early predictors of treatment response, according to a study presented at the San Antonio Breast Cancer Symposium (SABCS).
Researchers from the University of California, San Francisco (UCSF) presented preliminary findings from the American College of Radiology Imaging Network (ACRIN) 6657 trial, the largest trial ever conducted to examine the value of MRI in assessing response to neoadjuvant chemotherapy for breast cancer.
"We found that after just one cycle of preoperative chemotherapy, we can predict the likelihood that the patient will achieve a pathologic complete response [pCR]," said lead author Nola Hylton, Ph.D., the UCSF researcher who presented the data at the symposium.
"Of the MRI measurements, volume was the most predictive," she said. "Even in the multivariate analysis, change in volume was the only significant predictor of a pCR."
Achievement of a pCR has been well correlated with improved clinical outcomes, she noted. Mammography did not add value in this setting.
Her presentation was a preliminary analysis of 216 patients in ACRIN 6657, the imaging component of the I-SPY (Investigation of Serial Studies to Predict Your Therapeutic Response With Imaging and Molecular Analysis) trial, which is a multicenter study of patients with locally advanced breast cancer. I-SPY is integrating serial biopsy and MRI to quantitate breast tumor response to preoperative chemotherapy, in an attempt to identify surrogate markers that might predict pCR and survival. When response is determined early, treatment can be modified if necessary, and risk of recurrence can be estimated.
MRI assessments included tumor longest diameter, tumor volume, signal enhancement ratio, mammographic longest diameter, and clinical size.
At the time of analysis, 42 patients had progressed or died, with a mean time to progression of 21 months; 174 patients were progression-free at a mean time of 42 months.
At the t4 time point, MRI volume was more strongly correlated with pathology size than MRI tumor longest diameter, mammographic longest diameter, or clinical size (r = 0.61, versus 0.28, 0.24, and 0.43). Mammographic longest diameter was not correlated with pathological size of the tumor, Hylton reported.
In the multivariate model, MRI volume was the only early-change measurement at t2 to predict clinical response, carrying an odds ratio of 5.78 (p = 0.008), and to predict pCR, with an odds ratio of 1.94 (p = 0.011).
Hylton added that MRI volume can be generated in an automated fashion and was reproducible in this multicenter evaluation.
Ultimately, ACRIN investigators hope to observe a relationship between MRI volume change and survival. As it stands now, this end point gives "a relatively good gauge in the trajectory of treatment of where the patient is heading," she said. "It gives the medical oncologist confidence to change treatment when a poor response is observed."
More on MRI and neoadjuvant response
Accurate assessment of the extent of residual breast cancer after neoadjuvant chemotherapy is critical to surgical planning. Several other reports from the San Antonio meeting added to what is emerging on the value of MRI.
Preoperative MRI changed treatment decisions in 44% to 66% of patients 42 years of age or younger in a retrospective study of 32 women at Canadian centers. The most common change in surgical recommendation was from lumpectomy or quadrantectomy to mastectomy, due to finding more extensive disease, reported Dr. S.D. Mukherjee and colleagues from McMaster University in Hamilton, Ontario.
In another retrospective analysis, investigators from the Netherlands Cancer Institute in Amsterdam aimed to determine the accuracy of MRI in selecting patients for breast-conserving therapy (BCT) after neoadjuvant chemotherapy.
Of 130 patients treated with neoadjuvant chemotherapy, 61 patients (47%) were found to have a discrepancy of greater than 10 mm in tumor size imaged on MRI compared to size noted on the pathology report. For about half of these patients, this discrepancy would dictate a different surgical treatment.
Based on MRI indication for BCT, 19 of these 32 patients would have unjustly undergone BCT (disease extent at MRI less than 30 mm and disease extent at pathology greater than 30 mm), while for 13 patients, MRI alone would have led to mastectomy (extent greater than 30 mm) although the actual extent at pathology was less than 30 mm, reported Dr. M.E. Straver and colleagues.
MRI accurately selected the optimal treatment in 75% of patients. For the 25% of patients who were not correctly identified, MRI underestimated some and overestimated others. In multivariate analysis, histological subtype (lobular, ER-positive/HER2-negative) and type of lesion on baseline (diffuse) significantly influenced the accuracy of MRI to select patients for breast-conserving therapy.
By Caroline Helwick
AuntMinnie.com contributing writer
December 19, 2008
Related Reading
Rotating breast cancer tests helps high-risk women, December 15, 2008
Study: How well does MRI-guided breast biopsy work? December 5, 2008
MRI helps predict breast cancer invasiveness at surgery, December 1, 2008
Annual breast screening more effective than biennial, November 28, 2008
MRI beats mammo for gauging breast cancer treatment response, October 7, 2008
Copyright © 2008 AuntMinnie.com