GENEVA - Herniated lumbar disks aren't the most common back injury, but when they occur they often require surgery. And diagnosis requires tedious manual measurements -- or at least it did until researchers from London found a way to automate the process.
"Lower back pain is a major health concern with major effects on patients' quality of life, while at the same time it imposes tremendous costs on society, with costs exceeding $100 billion per year in the U.S. alone," said Sofia Michopoulou from University College London.
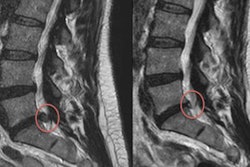
 |
| Intervertebral disk herniation is seen in the localized displacement of disk material beyond the limits of the intervertebral disk space -- either protrusion or extrusion. All images courtesy of Sofia Michopoulou. |
MRI is nearly ideal as a diagnostic tool for intervertebral lumbar disk herniation due to its excellent soft-tissue contrast, which enables precise delineation of the disk borders, said Michopoulou in a Friday presentation at the Computer Assisted Radiology and Surgery (CARS) meeting in Geneva.
Unfortunately, the diagnosis is a time-consuming process that "relies on qualitative descriptions of the disk boundaries, or semiquantitative disk measurements," and as a result suffers from moderately poor interobserver agreement (κ < 0.6), she said.
But hernia size does matter, especially for evaluating spontaneous regression and monitoring the disease process, she said. Surgery isn't always necessary -- sometimes conservative treatment can alleviate the symptoms or even eliminate the back pain and sciatica. But accurate diagnosis is essential for good patient management.
Because measurements are operator-dependent, clinicians are "sometimes hesitant to call it" herniation, she said. Therefore, her study sought to design an image analysis tool for the quantification and computer-aided diagnosis (CAD) of intervertebral disk herniation.
"The motivation is to provide a second reader to support the initial diagnosis and improve interobserver agreement," Michopoulou said. An automated tool would also help by providing accurate and repeatable measurements of hernia size and helping to monitor changes over time, in addition to reducing the need for tedious manual segmentation and measurements.
Michopoulou and colleagues examined 100 lumbar intervertebral disk studies from 20 T2-weighted MR images of the spine acquired on a 3-tesla MRI scanner (Signa, GE Healthcare, Chalfont St. Giles, U.K.). The multislice 2D data were acquired with a voxel size of 0.55 x 0.55 x 3 mm3, plus a 1-mm interslice gap, Michopoulou explained.
"The good thing is that [the studies] are readily available in clinical practice, but the bad thing is that they are 2D data, so we can't really get good volumetric information out of them," she said. Interpolation was used in some datasets to approximate 3D image data.
Ground truth for grading the extent of disease was provided by an experienced musculoskeletal radiologist who characterized the disks as normal or herniated (protrusion or extrusion) following the Nomenclature Project guidelines. In all, there were 71 normal disks, 21 protrusions, and eight extrusions in the cohort.
 |
| Lumbar disk segmentation in the study was based on a hybrid algorithm combining fuzzy clustering techniques with a probabilistic disk atlas. Shape and textural features were extracted from each segmented disk region to quantify its properties. |
The disks depicted on MRI were extracted from the rest of the dataset using an Atlas process. Then shape and textural features were extracted from each segmented disk region including region descriptors, Hu's moments, Fourier descriptors, first-order textural features, and co-occurrence features.
 |
| CAD segments the intervertebral disk material (right) from T2-weighted MR images. |
Measurement repeatability was tested using interclass correlation coefficients, and the research team used statistical analysis to probe the descriptive ability of the various features, Michopoulou explained.
The final step was quantification of the data features selection using stepwise discriminant analysis, classification by majority voting on the three classifiers, and CAD testing. The system was trained using the leave-one-patient-out validation method.
The CAD's sensitivity for detecting a herniated disk was 93%, with a specificity of 83%. The area under the receiver operator characteristics curve was 92%; agreement with the radiologist not using CAD was 69%.
"The CAD system segmentation algorithm delivered high accuracy with quantitative measurements from the automated system that are highly repeatable, and good agreement with the radiologist," Michopoulou said.
In other results, the algorithm showed highly accurate segmentation performance, with a mean boundary error of less than 1 mm that included both normal and herniated disks, Michopoulou said. Processing time was two seconds per disk for 2D data and 20 seconds per disk for the "pseudo-3D" interpolated data, Michopoulou said.
 |
| CAD output distinguishes normal from herniated lumbar disks. |
Measurement repeatability rose to an intraclass correlation coefficient greater than 0.97 using the method, and both regional features and co-occurrence textural features showed statistically significant differences between normal and herniated disks (p < 0.001).
The study is ongoing, with three radiologists currently testing the system to see if it supports their daily workflow in both diagnosis and assessing treatment response, she said. The system is also being trained to distinguish between protrusions and extrusions.
"So far, we have seen that the system has potential to support the clinical diagnosis of disk herniation. However, this hasn't been verified and it hasn't been tested yet on a second reader," Michopoulou said.
By Eric Barnes
AuntMinnie.com staff writer
June 28, 2010
Related Reading
Study questions routine x-rays, MRIs for back pain, February 6, 2009
MRI develops vital role in spinal evaluation, January 2, 2009
What do orthopedists want? In-office MRI, digital x-ray, report finds, March 28, 2007
MR overordered by primary physicians for back pain, January 31, 2006
Copyright © 2010 AuntMinnie.com