Dedicated ultrasound and MRI protocols -- in contrast to routine ones -- are more effective in diagnosing endometriosis, researchers have reported.
The results could lead to better patient care, noted a team led by Angela Tong, MD, of NYU Grossman School of Medicine in New York City. The group's findings were published September 11 in the American Journal of Roentgenology.
"Correct workup [of endometriosis] is imperative for timely diagnosis and can involve both ultrasound and MRI," it explained. "Knowing when to use which modality is important for efficient diagnosis and treatment planning."
Endometriosis affects 10% of women with symptoms of pelvic pain who are of childbearing age, Tong and colleagues wrote. Delay to diagnosis can average more than six years, and this delay not only results in "more difficulty for the patient but also increases endometriosis-related emergency visits." Yet whether ultrasound or MRI is most effective for assessing the condition has been uncertain.
To compare performance of the two modalities for this indication, the group conducted a review of 33 studies (culled from a total of 4,482 found on an initial publication search) that compared the efficacy of ultrasound and/or MRI in detecting endometriosis. Most of the research was performed at centers with significant experience with the condition, using dedicated rather than routine ultrasound and MRI protocols, the team explained.
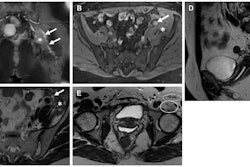
The dedicated ultrasound protocol was one for transvaginal ultrasound, which used a transducer of mid- to high frequency and allowed for higher spatial resolution. The dedicated MRI protocol for endometriosis included the following:
- T2-weighted turbo spin echo without fat-suppressed axial (including small field of view) and sagittal, with or without coronal views.
- T1-weighted gradient-echo in- and opposed-phase axial.
- Diffusion-weighted imaging and apparent diffusion coefficient mapping, axial.
- T1-weighted gradient-echo with fat suppression without IV contrast material, axial and sagittal, with or without coronal.
- T1-weighted gradient-echo with fat suppression, IV contrast, and subtraction.
- Axial and sagittal, with or without coronal.
- T2-weighted single shot fast spin echo, using a large field of view to include kidneys for evaluation of hydronephrosis.
The authors reported that, overall, routine ultrasound and MRI protocols had poorer performance than dedicated ones, which they suggested could lead to delays in diagnoses. They also found that ultrasound had better accuracy for identifying depth of wall invasion in bowel wall disease while MRI was better at visualizing pelvic wall and extraperitoneal disease.
Finally, when the group considered all the studies included in the review, weighted mean sensitivities for detecting endometriomas on ultrasound was 81% and on MRI, 67.8%. The weighted mean specificity for ultrasound was 84.4% and 83.2% for MRI.
The bottom line? Clinicians should choose which modality to use to diagnose endometriosis depending on available expertise and keep in close contact with their gynecology peers, according to Tong's team.
"If both [modalities] are available, performing MRI first may allow better assessment of the full extent of intraperitoneal and extraperitoneal disease," the group concluded. "Follow-up dedicated ultrasound may be performed to further interrogate areas of disease and inform comprehensive treatment planning. Consistent communication between radiology and gynecology professionals is recommended to … provide the best care for patients."
The complete study can be found here.