A new scoring model for MRI exams shows potential for improving the assessment of early recurrence in patients with hepatocellular carcinoma (HCC), according to a study published February 11 in Radiology.
The model is based on gadoxetic acid-enhanced MRI scans and includes a practical “image score” that could help clinicians implement more effective interventions, noted lead authors Kun Zhang, MD, of Nankai University, and Kan He, MD, of the First Hospital of Jilin University, both in China.
“A comprehensive noninvasive preoperative analysis of high-risk pathologic features would be valuable for facilitating informed treatment decision-making and improving the prognosis of patients with HCC,” the group wrote.
Radical surgery is the primary treatment for HCC, but early recurrence remains a significant challenge, given that pathologic analysis of HCC is invasive and complicated and that results are sometimes incomplete, the authors explained.
Alternatively, they noted that recent studies have confirmed the merits of scoring models based on clinical data and imaging features. However, scoring models based on gadoxetic acid-enhanced MRI features for predicting pathologic indicators in HCC are scarce, they wrote.
Hence, to develop a model, the researchers collected data from 366 patients with HCC who underwent preoperative gadoxetic acid-enhanced MRI at three centers between January 2014 and January 2021.
The group evaluated preoperative imaging characteristics of each patient using pathological specimens as the reference standard and identified five imaging features associated with high-risk pathologic features: diameter greater than 4 cm, irregular morphology, intratumoral arteries, peritumoral enhancement in the arterial phase, and low peritumoral signal intensity.
Next, based on these imaging features, the researchers developed a score called the Image score (I-score) and tested its ability to predict early recurrence of HCC on a training dataset (n = 150), two external validation datasets (n = 73 and n = 56), and an outcome dataset (n = 87).
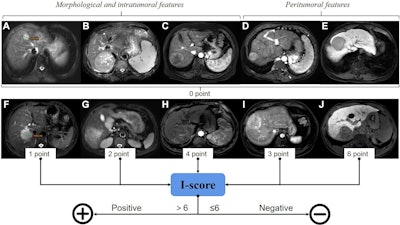 Assignment of the Image score (I-score) based on imaging features assessed on axial gadoxetic acid-enhanced MRI scans. (A–E) Imaging features representing zero points: (A) maximum tumor diameter (TD-max) of 4.0 cm or less, (B) regular shape, (C) no intratumoral arteries (ITAs), (D) no peritumoral enhancement in the arterial phase, and (E) absence of low peritumoral signal intensity in the hepatobiliary phase. (F–J) Imaging features representing added points: (F) one point for TD-max greater than 4 cm, (G) two points for irregular morphology, (H) four points for ITAs, (I) three points for peritumoral enhancement in the arterial phase, and (J) six points for low peritumoral signal intensity in the hepatobiliary phase. The features were assessed, and a scoring model with continuous I-score was established to evaluate high-risk pathologic features in hepatocellular carcinoma. The threshold value of the I-score obtained via receiver operating characteristic curve analysis was used to predict high-risk pathologic features. When the I-score was greater than 6, it was considered positive; otherwise, it was considered negative. TD-max and morphology can also be assessed on T2-weighted images. Image and caption courtesy of RSNA.
Assignment of the Image score (I-score) based on imaging features assessed on axial gadoxetic acid-enhanced MRI scans. (A–E) Imaging features representing zero points: (A) maximum tumor diameter (TD-max) of 4.0 cm or less, (B) regular shape, (C) no intratumoral arteries (ITAs), (D) no peritumoral enhancement in the arterial phase, and (E) absence of low peritumoral signal intensity in the hepatobiliary phase. (F–J) Imaging features representing added points: (F) one point for TD-max greater than 4 cm, (G) two points for irregular morphology, (H) four points for ITAs, (I) three points for peritumoral enhancement in the arterial phase, and (J) six points for low peritumoral signal intensity in the hepatobiliary phase. The features were assessed, and a scoring model with continuous I-score was established to evaluate high-risk pathologic features in hepatocellular carcinoma. The threshold value of the I-score obtained via receiver operating characteristic curve analysis was used to predict high-risk pathologic features. When the I-score was greater than 6, it was considered positive; otherwise, it was considered negative. TD-max and morphology can also be assessed on T2-weighted images. Image and caption courtesy of RSNA.
According to the results, in the training dataset, the model achieved “excellent performance” for predicting high-risk pathologic features, with an area under the receiver operating characteristic curve (AUC) of 0.93. In the two external validation datasets, the model also exhibited excellent performance, with AUCs of 0.86 and 0.84, indicating high accuracy.
In the outcome dataset, a combined model that incorporated the I-score along with two other predictors demonstrated better prognostic performance, with a concordance index of 0.84, the group reported.
“The novel scoring model presented here has the potential to improve the assessment of early recurrence in patients with HCC,” the researchers wrote.
Ultimately, many studies have developed methods for predicting pathologic features in HCC, yet most previous studies were limited to the study of one pathologic feature, rather than integrating multiple pathologic features, the group noted. Moreover, the model performed well despite being developed and tested in patients from different geographic regions and treated in different hospitals, they added.
Nonetheless, the further validation is needed, they wrote.
“Additional validation studies involving larger and more diverse patient datasets are needed to confirm the clinical utility of the scoring model and evaluate its performance across different stages of HCC,” the researchers concluded.
The full study is available here.