Intracardiac reconstructive surgery can be used to repair defects in the beating heart while avoiding the need for cardiopulmonary bypass. But progress in the advanced interventional technique has been limited by a lack of reliable imaging tools.
A study appearing today in the Journal of Thoracic and Cardiovascular Surgery introduces a solution based on video gaming technology to improve the results of real-time 3D echocardiography (RT3DE).
Standard real-time 3D echocardiography, which provides good visualization of cardiac anatomy while enabling navigation of surgical instruments toward targets inside the beating heart, has been shown to be a viable tool for guiding interventions.
To perform RT3DE safely, however, the surgeon has to visualize and manipulate rapidly moving anatomic structures inside a beating heart, relying on real-time visual feedback. Current tools need improvement, wrote the authors, who included Nikolay Vasiliyev; Dr. Paul Novotony, Ph.D.; Dr. Pedro del Nido; and colleagues from Children's Hospital Boston and Harvard Medical School in Boston (Journal of Thoracic and Cardiovascular Surgery, June 2008).
"In current systems, acquired ... 3D volume data are projected on a conventional 2D display where the depth of field is rendered by varying shades of gray. Therefore, while operating under RT3DE guidance, the surgeon may not have an adequate display of intracardiac structures in 3D space, and must rely on indirect evidence for depth perception and position of the instruments within the heart," they explained.
The study, funded by the National Institutes of Health, demonstrated good results based on simple technology borrowed from the gaming industry: stereo glasses.
In order to use real-time 3D echo data for guiding surgery, the researchers streamed data to an external computer, rendering volumetric datasets in real time to generate offset images on a stereoscopic vision display. The study sought to determine whether a custom-built display could improve the performance of RT3DE-guided surgery to repair atrial septal defects in an animal model.
The display technology for the stereoscopic glasses was designed to render 30 MB of data per second, using the computational power of consumer-level graphics processing units, Vasiliyev et al explained.
The programmable processing units can execute highly parallelized per-vertex and per-pixel user routines called shaders, they explained. In this process, pixel shaders are used to cast rays through the volumetric dataset in a ray-per-pixel method in which intensity and opacity are compounded by sampling the volumetric dataset along the projection ray.
The renderer was implemented on a DirectX 9.0c platform using the Pixel Shader 3.0 API on a GeForce FX 7800 (Nvidia, Santa Clara, CA). Hardware loops allowed for implementation of the sampling process in a single pass, maintaining interactive frame rates of at least 70 frames per second.
RT3DE data were obtained using an X4 matrix transducer on a Sonos 7500 ultrasound system (Philips Healthcare, Andover, MA). Typical streaming volumes of 128 x 48 x 204 voxels were produced at 25 Hz and sent with the aid of a transmission control protocol.
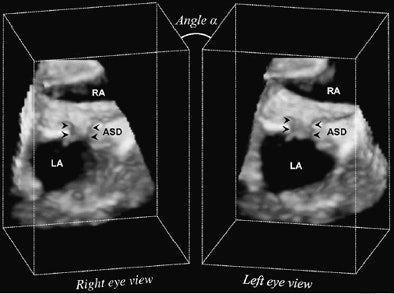 |
| The volumetric dataset of the created ASD (arrowheads) is sampled using parallel projection. Rays are cast simultaneously in a front-to-back fashion through the 3D ultrasound data. Left-eye and right-eye views are separately generated by rendering the 3D ultrasound volume from two viewpoints skewed by angle A. LA = left atrium; RA = right atrium. Image published with permission of the Journal of Thoracic and Cardiovascular Surgery. |
Under 3D echocardiography guidance, the group created 6-mm atrial septal defects in six pigs. They closed the defects with the aid of a catheter-based patch delivery system, attaching the patches with tissue minianchors.
The study compared 3D echocardiography with stereoscopic vision display to 3D echocardiography with standard display for guidance of the surgical repair process. Task performance measures for each anchor placement (32 anchors per group) included completion time, trajectory of the tip of the anchor deployment device, and accuracy of the anchor placement.
The results showed that the mean anchor deployment time in the stereoscopic vision display group was shorter by 44% compared to the standard display group: 9.7 ± 0.9 seconds versus 17.2 ± 0.9 seconds (p < 0.001), Vasiliyev and his colleagues wrote.
The tip of the anchoring deployment device was also navigated more accurately with use of the glasses. Deviation from the ideal path averaged 3.8 mm compared to 6.1 mm, a 38% improvement.
However, accuracy of the anchor placement was the same for both methods at 2.3 ± 0.3 mm for the stereoscopic vision display procedures versus 2.3 ± 0.3 mm for the standard display procedures.
"In our series, all the experiments were done by an operator who had significant experience with beating-heart intracardiac 3D echocardiography (3DE)-guided procedures," the authors wrote. "This may explain why there was no significant advantage of [stereoscopic vision] display in accuracy of anchor placement when compared with the 2D display."
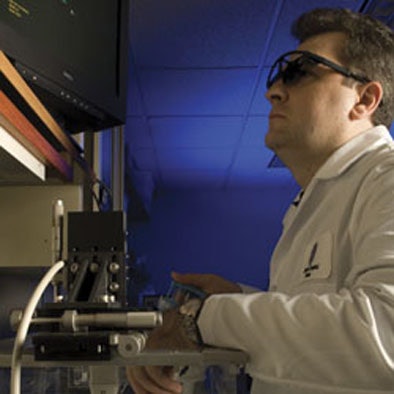 |
| Dr. Nikolay Vasiliyev practices anchoring an atrial patch under 3D stereoscopic guidance. Image by Bill O'Connell published with permission of the Journal of Thoracic and Cardiovascular Surgery. |
Real-time 3D is needed to control and navigate surgical instruments and repair defects in the heart due to the need to "recognize and manipulate delicate cardiac tissues within a rapidly moving and geometrically complex structure," they wrote.
Surgeons who perform endoscopic procedures are trained to "base their judgments as to instrument navigation and tissue manipulation primarily on direct vision via optical endoscopic imaging," they wrote. "However, ultrasound imaging does not have the spatial resolution of optical imaging, and therefore the ability of the surgeon to identify surgical instruments and instrument position with respect to the target tissue is more limited."
While the spatial resolution of 3D ultrasound systems has improved significantly in the last several years, the lack of fine detail complicates interpretation of the depth of field.
"The usual cues used by endoscopic surgeons to provide positional information of instruments within the field-of-view are not readily available with [standard] 3D US imaging," they wrote.
The study confirmed the group's hypothesis that stereoscopic displays would provide better spatial information and depth perception, improving results significantly even for an experienced endoscopic surgeon, they wrote.
Stereoscopic vision systems for echocardiography were first introduced a decade ago with mixed results; however, visualization systems -- as well as ultrasound technology -- have improved in the interim.
A principal limitation of the study was that the experiments were performed by a single experienced surgeon. However, a previous experiment performed with 16 subjects with varying experience in endoscopic surgery and the same visualization system yielded a 28% improvement in task completion times and a 50% reduction in error rates.
"Stereoscopic vision display combined with 3D echocardiography improved the visualization of 3D echocardiography ultrasound images, decreased the time required for surgical task completion, and increased the precision of instrument navigation, potentially improving the safety of beating-heart intracardiac surgical interventions," the authors concluded.
By Eric Barnes
AuntMinnie.com staff writer
June 9, 2008
Related Reading
Giant virtual reality chamber boosts 3D echo accuracy, August 2, 2007
Cardiac CT drives adoption of 3D visualization, March 26, 2007
Virtual human puts doctors inside their patients, May 24, 2007
Survey finds routine use of 3D visualization, December 18, 2006
Part III: Image processing has room to grow, October 23, 2006
Copyright © 2008 AuntMinnie.com