Microultrasound may be a suitable alternative to MRI for image-guided prostate biopsy, suggest findings published March 23 in JAMA.
Microultrasound’s performance was noninferior to that of MRI and conventional ultrasound in a randomized clinical trial led by Adam Kinnaird, MD, PhD, from the University of Alberta in Edmonton, Alberta, Canada, and colleagues. This finding applied to fusion-guided biopsy for finding intermediate or higher grades of prostate cancer in men who have not previously undergone biopsy.
“For patients and physicians, microultrasonography is a novel method of imaging and biopsy with potential greater accessibility for patients considering prostate biopsy, particularly for patients with contraindications to MRI,” the Kinnaird team wrote.
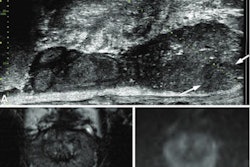
Microultrasound has emerged as an alternative imaging method that uses high-energy sound waves to create images that proponents say are more detailed than conventional ultrasound. It yields an imaging resolution of 70 microns, which is the diameter of a typical prostate duct.
As part of the Optimum randomized clinical trial, Kinnaird and co-authors compared the performance of microultrasound (ExactVu, Exact Imaging) to that of conventional MRI and ultrasound during biopsy for detecting clinically significant prostate cancer. They also investigated whether a combination approach via microultrasound and MRI for fusion-guided biopsy would perform better than that of conventional combined approaches.
Final analysis included data collected from 20 centers for 802 men with a median age of 65. Of the total, 678 underwent biopsy. The median prostate-specific antigen level among the patients was 6.9 ng/mL.
Of the total patients, 137 were randomized to microultrasound only, 402 to the MRI and conventional ultrasound group, and 263 to the microultrasound and MRI group.
The team focused on Gleason Grade Group 2 or higher prostate cancers. Microultrasound found these cancers in 57 patients (47.1%), combined MRI and conventional ultrasound detected 141 (42.6%), and microultrasound combined with MRI found 106 cancers (46.9%).
Microultrasound-guided biopsy proved to be noninferior to MRI fusion-guided biopsy, with a difference of 3.5% in detecting clinically significant prostate cancer (noninferiority, p < 0.001). Combined biopsy with microultrasound and MRI was also noninferior to MRI and conventional ultrasound software-assisted MRI fusion biopsy using conventional ultrasound devices. This included a difference of 4.3% in finding clinically significant cancers (noninferiority, p < 0.001).
Finally, the rates of cancers deemed to be Gleason Grade Group 2 or higher that were diagnosed by targeted biopsy only included the following: 38% in the microultrasound group; 34.1% in the MRI and conventional ultrasound group; and 40.3% in the microultrasound and MRI group. The researchers reported that these differences did not achieve statistical significance.
The study authors highlighted that using microultrasound in this area can reduce wait times, cost, contrast-related morbidity, and patient anxiety. This is due to microultrasound not requiring contrast use. The authors added that this could also lessen the need for prebiopsy MRI with contrast.
“For regions with limited MRI access, microultrasonography represents an imaging and biopsy technique that omits the accessibility and resource limitations of MRI capabilities,” they wrote. “This has particular importance given the predicted increase in prostate cancer incidence and limited MRI capacity worldwide.”
The full study can be found here.