ORLANDO – A 3D-printed simulation model could help improve ultrasound-guided anesthesia, according to results presented March 31 at the 2025 American Institute of Ultrasound in Medicine (AIUM) annual conference.
In his presentation, Erick Torres, MD, from the University of California, San Diego showed his team’s work in creating the model, which significantly improved the skills of emergency physicians in accurately administering ultrasound-guided regional anesthesia.
“This model showed that feedback did improve needle targeting,” Torres said. “It’s a promising simulation for ultrasound-guided regional anesthesia.”
Ultrasound-guided regional anesthesia helps emergency physicians achieve analgesia, but it requires precision to avoid damaging nerves or structures surrounding the target area of administration.
Simulation models teach physicians the essentials of proficient anesthesia administration under ultrasound guidance. However, Torres highlighted that many models are expensive and don’t provide immediate feedback for correct needle placement.
Torres and colleagues developed their own simulation model to address these concerns, using 3D printing to help replicate a fascial plane block. They also placed two standing rectangular blocks to mimic ribs, serving as obstacles that physicians may face in real-world situations. The model used electrical circuitry connected to a metal ball bearing, which appeared as an echogenic target on ultrasound. The team filled the 3D-printed base with Humimic ballistic gel to mimic human skin and soft tissue.
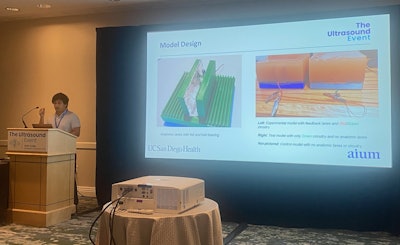 Erick Torres, MD, describes a 3D-printed simulation model he and colleagues created, which results show marked improvement in accurate needle targeting among medical students and residents performing ultrasound-guided regional anesthesia.
Erick Torres, MD, describes a 3D-printed simulation model he and colleagues created, which results show marked improvement in accurate needle targeting among medical students and residents performing ultrasound-guided regional anesthesia.
Trainees positioned the needle to target the ball bearing. If they correctly positioned it, they were notified immediately via a green LED light. A red LED light meanwhile meant the needle was not correctly positioned.
In total, the researchers created three models: one with feedback circuitry and anatomic lanes, one that provided a green LED light only, and another that had no feedback circuitry or anatomic lanes. The no-feedback model served as the control for the team’s study.
Forty-nine medical students and residents of varying experience levels participated in the study. Of these, 28 worked on the models that provided immediate feedback while 21 worked on the control model.
The immediate feedback group improved their procedure time by 40.3% on average while the control group’s time worsened by 12.6% (p < 0.05).
On a 1- to 5-point helpfulness rating (5 being most helpful), the immediate feedback group rated the model at 4.71 on average, compared to 3.95 for the control group (p = 0.001). And while comfort with the ultrasound procedure increased in both groups, this finding did not achieve statistical significance.
Torres said future analyses could explore trends in incorrect needle placement and how different materials for mimicking anatomic lanes or other ballistic gels may impact performance.
“And then we do this more longitudinally as medical trainees go on with their experiments and see if they improve,” he added.