Areas with high levels of social-environmental injustice (SEI) experience lower rates of cancer screening, according to research published on September 16 in JAMA Network Open.
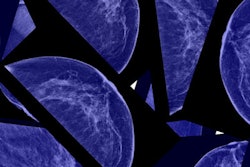
A team led by Kilan Ashad-Bishop, PhD, from the University of Miami in Coral Gables, FL, found that these SEI "hot spots" -- geographic areas with high SEI -- had the lowest prevalence of all screening modalities. Additionally, breast cancer screening prevalence relative to non-hot spots was larger in SEI hot spots than in hot spots that have just social vulnerability or just environmental burden.
"Structural inequity and environmental injustice in the U.S. have patterned cancer disparities, particularly along racial and socioeconomic lines, while reducing the ability of affected communities to avoid these negative health outcomes," the Ashad-Bishop team wrote.
Previous studies suggest that environmental injustice, characterized by poor or marginalized communities being harmed by hazardous waste, resource extraction, and other land uses, is tied to elevated risk of cancer incidence and mortality. Also, previous studies have described the relationship between social risk factors and cancer.
The researchers noted a lack of cancer control studies assessing socially at-risk communities being affected by environmental injustice.
Ashad-Bishop and co-authors used an environmental injustice index to characterize the prevalence of cancer screening across geographic clusters influenced by social risk factors and environmental burden. They also did this for compounded social-environmental injustice factors in densely populated urban areas.
The team used unweighted percentile-ranked sums of the social and environmental indicators from the 2022 release of the U.S. Centers for Disease Control and Prevention Environmental Justice Index. Ashad-Bishop and colleagues then used the index to quantify census tract-level exposures of social vulnerability and environmental burden, including model-based estimates of breast, cervical, and colorectal cancer screening as dictated by recommendations from the U.S. Preventive Services Task Force.
The researchers analyzed 7,791 census tracts and found that 410 (5.3%) were SEI hot spots, with the highest prevalence of these found in western U.S. counties such as Los Angeles and Maricopa in Arizona.
SEI hot spots experience the lowest average prevalence of cancer screening relative to hot spots of social vulnerability alone and environmental burden alone.
| Average prevalence of cancer screening relative to hot spots | |||
|---|---|---|---|
| Cancer screening | Social vulnerability alone | Environmental burden alone | SEI |
| Breast | 78.1% | 78.1% | 76.6% |
| Cervical | 79.1% | 81.3% | 78.4% |
| Colorectal | 53% | 59% | 51% |
Also, the prevalence difference for mammography between hot spots (76.6%) and non-hot spots (78.5%) of SEI was 1.9 percentage points. To compare, the prevalence difference between hot spots and non-hot spots of social vulnerability alone and environmental burden alone was 0.3 percentage points.
The team also observed significantly lower mammography prevalence among SEI hot spots relative to non-hot spots in Los Angeles County, CA; Harris County, TX; Philadelphia County, PA; and Maricopa County, AZ.
Finally, the researchers found lower prevalence differences for cervical and colorectal cancer screening in SEI hot spots (4.1 percentage points) compared to non-hot spots (10.6 percentage points).
The study authors suggested that identifying areas of greatest SEI can help in the development of place-based cancer control efforts, which could take into account structural indicators associated with lower mammography participation alongside direct efforts at bolstering access to breast cancer screening, they added.
The full study can be found here.