Hormonal effects influence the degree of background parenchymal enhancement (BPE) on contrast-enhanced mammography (CEM), suggest findings published February 11 in Radiology.
Researchers led by Noam Nissan, MD, PhD, from Memorial Sloan Kettering Cancer Center in New York found that menopausal status, lactation, hormone replacement therapy (HRT), and tamoxifen therapy affect the degree of BPE, an imaging biomarker, on CEM exams.
“Our results highlight higher BPE in premenopausal compared with post-menopausal female patients, increased BPE during lactation and hormone replacement therapy, and decreased BPE during tamoxifen therapy, which increased at treatment cessation,” Nissan and co-authors wrote.
BPE is an important diagnostic and prognostic biomarker, with a higher degree BPE on imaging being tied to a higher likelihood of developing breast cancer.
Previous studies have investigated hormonal regulation of BPE on breast MRI, though information is lacking for CEM, the researchers noted. They studied how BPE at CEM changes across various short- and long-term physiologic and pharmacologic hormonal effects.
The retrospective study included data collected between 2012 and 2024 from 507 women with an average age of 49.8 years. These women underwent CEM and had varying hormonal statuses. The researchers placed women in one or more of several subgroups, including the following: premenopausal, postmenopausal, lactating, HRT, and tamoxifen. For women who received tamoxifen therapy, the team included the first follow-up image at treatment cessation, when available.
The researchers observed the following:
- Premenopausal women (n = 200) had higher BPE (median grade, 1) compared with postmenopausal women (n = 200, median grade, 0; p < 0.001).
- Lactating women (n = 16) showed higher BPE (median grade, 3) compared with nonlactating women (median grade, 1; p < 0.001).
- Women receiving HRT (n = 14) showed higher BPE (median grade, 1.5) compared with postmenopausal women (median grade, 0; p < 0.001).
Finally, women receiving tamoxifen therapy (n = 77) had lower BPE than nontreated women. This included a median BPE grade of 1 for women undergoing HRT. Of the total, 9% of women undergoing tamoxifen therapy had higher BPE compared to 31% of nontreated women (p < 0.001). When therapy ceased, women had increased BPE at a median grade of 2 (p = 0.003).
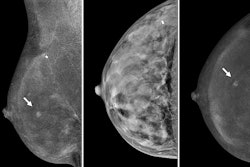
 Images depict ongitudinal background parenchymal enhancement (BPE) changes at contrast-enhanced mammography (CEM) related to tamoxifen therapy and cessation. Recombined (A, B) left and (C, D) right mediolateral oblique CEM images in two different 51-year-old female patients who underwent imaging while receiving tamoxifen therapy (A, C) and after cessation of therapy (B, D) show minimal BPE during tamoxifen therapy, which increased to marked and moderate BPE grades, respectively, after cessation.Images and caption courtesy of the RSNA.
Images depict ongitudinal background parenchymal enhancement (BPE) changes at contrast-enhanced mammography (CEM) related to tamoxifen therapy and cessation. Recombined (A, B) left and (C, D) right mediolateral oblique CEM images in two different 51-year-old female patients who underwent imaging while receiving tamoxifen therapy (A, C) and after cessation of therapy (B, D) show minimal BPE during tamoxifen therapy, which increased to marked and moderate BPE grades, respectively, after cessation.Images and caption courtesy of the RSNA.
The study authors highlighted that their findings add to the complexity of understanding the nature of BPE, “as it is a dynamic rather than constant factor.”
“To minimize further diagnostic interventions, it is crucial to understand its hormonal modulation and how it uniquely manifests in the subgroups studied,” they wrote. “Familiarity with these variations can help radiologists make more accurate interpretations and reduce unnecessary follow-ups.”
The authors also called for future research to explore the impact of these hormonal alterations on the diagnostic performance of CEM.
In an accompanying editorial, Priscilla Slanetz, MD, from Boston Medical Center and Boston University in Massachusetts wrote that more research is needed on CEM and BPE to find out the best ways to measure BPE on breast imaging and BPE’s role in breast cancer risk. She also highlighted how machine learning could aid in these areas and whether BPE at CEM will act similarly to MRI in predicting cancer risk and response to neoadjuvant chemotherapy.
“By understanding the factors that influence BPE at CEM, radiologists will be able to provide more accurate interpretations and make more informed management decisions, thereby providing optimal life-saving patient care,” Slanetz wrote.
The full study can be accessed here.