Imaging surveillance may be a safe alternative to surgical excision for architectural distortions detected by digital breast tomosynthesis (DBT) alone, suggest findings published March 12 in the American Journal of Roentgenology.
Researchers led by Derek Nguyen, MD, from Duke University in Durham, NC, found that for architectural distortions found by DBT alone with no ultrasound correlate, the malignancy rate was 0% for distortions without atypia versus 20% for distortions with atypia on core needle biopsy.
“Our study found that imaging surveillance may be a safe alternative to surgical excision for architectural distortions detected by DBT alone, without an ultrasound correlate, when core needle biopsy demonstrates benign pathology, including radial scars without atypia,” Nguyen told AuntMinnie.com.
Previous reports indicate that architectural distortions found on DBT images are more often tied to nonmalignant pathologies than those detected on digital mammography. Core needle biopsy is the go-to management method for these distortions since the malignancy risk is still high.
The Nguyen team studied outcomes of architectural distortions found by DBT alone with no ultrasound correlate. This included evaluating their relationship with non-malignant results on core needle biopsy. The group's goal was to decide the best course of action when incorporating surveillance imaging with management strategies.
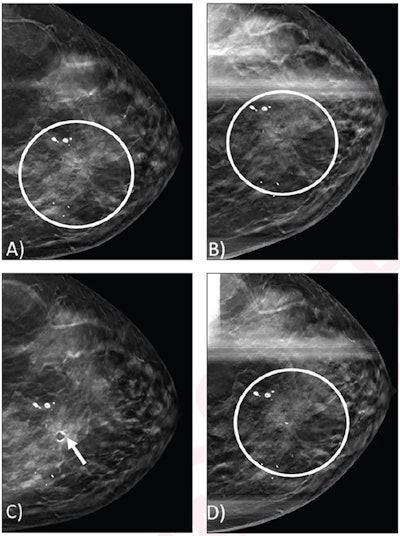 (A) Craniocaudal view from screening DBT mammogram shows architectural distortion (circle) in the upper inner position, which was not detected by digital mammography (not shown). (B) Spot craniocaudal view from subsequent diagnostic DBT mammogram shows persistence of architectural distortion (circle). No ultrasound correlate was identified (not shown). Core needle biopsy of the architectural distortion was performed, yielding a radial scar without atypia. (C) Post-biopsy mammogram shows cylinder clip (arrow) in appropriate position. Biopsy result was considered concordant, and patient underwent recommended imaging surveillance. (D) Spot craniocaudal view from diagnostic mammogram performed 12 months later shows stable appearance of an architectural distortion (circle).ARRS
(A) Craniocaudal view from screening DBT mammogram shows architectural distortion (circle) in the upper inner position, which was not detected by digital mammography (not shown). (B) Spot craniocaudal view from subsequent diagnostic DBT mammogram shows persistence of architectural distortion (circle). No ultrasound correlate was identified (not shown). Core needle biopsy of the architectural distortion was performed, yielding a radial scar without atypia. (C) Post-biopsy mammogram shows cylinder clip (arrow) in appropriate position. Biopsy result was considered concordant, and patient underwent recommended imaging surveillance. (D) Spot craniocaudal view from diagnostic mammogram performed 12 months later shows stable appearance of an architectural distortion (circle).ARRS
The retrospective study included 106 women with an average age of 58 years and 109 architectural distortions found on DBT. The women underwent either repeat core needle biopsy, surgical excision, or 12 months of diagnostic imaging follow-up. Biopsy was performed via 12 vacuum-assisted 9-gauge cores.
Clinicians recommended that women undergo surgical excision if their architectural distortion findings on DBT showed atypia. However, the women could electively undergo alternative management options. If no atypia was found, the women were recommended to undergo six-month and 12-month diagnostic imaging follow-up before returning to annual screening.
Overall, the malignancy rate was 0% (0 of 94) when atypia was not found versus 20% (three of 15) when atypia (with or without radial scar) was present on biopsy, the team reported.
| Malignancy rates for architectural distortions found on DBT | |
|---|---|
| Architectural distortion findings | Malignancy rate |
| Showing benign pathology on biopsy | 0% |
| Showing radial scar without atypia on biopsy | 0% |
| Showing radial scar with atypia on biopsy (all with excision) | 10% |
| Showing atypia without radial scar on biopsy | 40% |
Finally, all architectural distortions that underwent imaging surveillance were stable on 12-month diagnostic imaging follow-up and returned to routine annual screening. Of the distortion cases that returned to routine annual screening, 73% (16 of 22) had an available subsequent annual screening mammogram, showing stability in all cases. In the 14 distortions that underwent surgical excision, excision did not yield atypia or malignancy in any case.
Nguyen said that the variation in upgrade rates among different types of atypia highlights the need to consider the specific type of atypia when making management decisions, rather than applying a uniform approach to all cases.
The study authors highlighted that their findings support surveillance imaging as “a reasonable alternative” to surgery when atypia is not present while surgery is needed for when atypia is found.
“This may help refine clinical management strategies and reduce unnecessary surgical excisions while maintaining high standards of patient care,” Nguyen told AuntMinnie.com.
In an accompanying editorial, Aurela Clark, MD, from the University of Kentucky in Lexington wrote that the research team’s approach provides a reliable method that may reduce overtreatment and improve resource allocation.
“Mindful of optimizing patient care, individualized risk stratification should be considered to assess the need for risk-reducing interventions and supplemental breast MRI,” she added.
The full study can be found here.