Using the upcoming version of BI-RADS for auditing preoperative breast MRI is feasible, according to research published October 14 in Radiology.
A team led by Ethan Cohen, MD, from The University of Texas M.D. Anderson Cancer Center in Houston also reported that going by the soon-to-be-released BI-RADS manual resulted in metrics that were within expected ranges based on limited prior data.
“Automation of this process is essential to develop the robust benchmarks necessary for preoperative breast MRI quality assurance,” the Cohen team wrote.
The BI-RADS version 2025 manual will recommend auditing breast MRI exams performed to evaluate the extent of disease in newly diagnosed breast cancer cases. The proposed audit includes four calculations: abnormal interpretation rate (AIR), positive predictive value of biopsies recommended (PPV2), positive predictive value of biopsies performed (PPV3), and additional cancer detection rate.
While prior studies have estimated these metrics for preoperative MRI, the researchers noted a lack of data that included all four of the recommended audit calculations.
Cohen and colleagues studied the feasibility of the proposed audit by using preoperative breast MRI exams performed in 2021 and 2022. They also reported the calculated metrics and identified any clinical or imaging characteristics tied to improved MRI performance metrics.
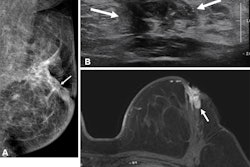
 Images in a 39-year-old woman with a remote history of right breast cancer and a new diagnosis of multicentric left breast cancer; this case illustrates appropriate auditing of true- and false-positive results. (A) Axial T1-weighted postcontrast image from preoperative breast MRI shows a small invasive mammary carcinoma with biopsy clip susceptibility artifact (circle) in the lateral left breast that was diagnosed before MRI. (B) Axial T1-weighted postcontrast image from the same examination reveals a smaller invasive mammary carcinoma with biopsy clip susceptibility artifact (circle) in the medial left breast that was also diagnosed before MRI. For the purpose of auditing in this study, the larger of these two malignancies was considered the index malignancy. (C) Axial T1-weighted postcontrast image from the same examination demonstrates an additional small mass in the posterior aspect of the left breast (circle). It was described as suspicious, and a third focus of invasive mammary carcinoma was diagnosed at MRI-guided biopsy. This pathologic result was audited as a true-positive ipsilateral finding. (D) Axial T1-weighted postcontrast image from the same examination shows a fourth mass in the contralateral right breast (circle), which was also described as suspicious. MRI-guided biopsy yielded benign fat necrosis and stromal fibrosis, which was audited as a false-positive contralateral finding.RSNA
Images in a 39-year-old woman with a remote history of right breast cancer and a new diagnosis of multicentric left breast cancer; this case illustrates appropriate auditing of true- and false-positive results. (A) Axial T1-weighted postcontrast image from preoperative breast MRI shows a small invasive mammary carcinoma with biopsy clip susceptibility artifact (circle) in the lateral left breast that was diagnosed before MRI. (B) Axial T1-weighted postcontrast image from the same examination reveals a smaller invasive mammary carcinoma with biopsy clip susceptibility artifact (circle) in the medial left breast that was also diagnosed before MRI. For the purpose of auditing in this study, the larger of these two malignancies was considered the index malignancy. (C) Axial T1-weighted postcontrast image from the same examination demonstrates an additional small mass in the posterior aspect of the left breast (circle). It was described as suspicious, and a third focus of invasive mammary carcinoma was diagnosed at MRI-guided biopsy. This pathologic result was audited as a true-positive ipsilateral finding. (D) Axial T1-weighted postcontrast image from the same examination shows a fourth mass in the contralateral right breast (circle), which was also described as suspicious. MRI-guided biopsy yielded benign fat necrosis and stromal fibrosis, which was audited as a false-positive contralateral finding.RSNA
The study included 1,533 preoperative MRI exams with a median patient age of 55. Of the total exams, 464 showed 609 suspicious breast imaging findings. Image-guided biopsy that followed for 432 of these findings revealed 139 malignancies.
The team reported the following:
The overall abnormal interpretation rate was 30.3%, PPV2 was 22.8%, PPV3 was 32.2%, and the additional cancer detection rate was 90.7 per 1,000 exams.
Seven radiologists spent a combined total of 141 hours collecting data and performing audit calculations.
Older patient age (odds ratio, 1.04; p < 0.001) and presence of lesions ipsilateral to the index malignancy (odds ratio, 1.81; p = 0.005) were associated with higher odds of malignancy.
The results highlight the need for preoperative MRI exams to be easily identifiable to allow for large-scale auditing, the study authors highlighted.
“We recommend adding a ‘Preoperative [or Staging] MRI’ label to the examination title in the medical record, imaging report, or both to facilitate accurate selection,” they wrote.
The authors also called for standardized definitions for preoperative MRI and for excluding MRI exams staging other breast malignancies from the audit. They also wrote that automating the auditing process “is the first step toward establishing reliable benchmarks for preoperative MRI audits.”
Read the full study here.