An old adage says practice makes perfect. But does it always? Perhaps not in breast imaging, say researchers who are studying the impact of raising the annual volume requirement for reading mammograms.
Under the Mammography Quality Standards Act (MQSA), U.S. radiologists are required to read a minimum of 960 mammograms within a two-year period (480 per year) to be certified to interpret mammography. As the belief that higher interpretation volumes bring increased accuracy gains hold, however, a push to raise this minimum has developed; advocates of this position cite annual volumes in other countries such as the U.K., Canada, and Australia, which are five to 10 times higher than the U.S. requirement.
Yet raising the volume requirement for interpreting mammography exams may have an unexpected result, according to Dr. Rebecca Smith-Bindman of the department of radiology at the University of California, San Francisco, and colleagues. If the annual mammography volume requirement for certification were raised, some U.S. radiologists -- particularly those practicing in rural settings -- would no longer read enough exams to stay certified, impacting patients' access to care.
The researchers sought to document the annual volume of mammography exams radiologists interpret, to therefore estimate the proportion of mammograms interpreted by radiologists in different volume categories. Their results were published in the American Journal of Roentgenology (February 1, 2008, Vol. 190, No. 2, pp. 526-532).
The group used data collected from mammography facilities that are part of the Breast Cancer Surveillance Consortium (BCSC), funded by the National Cancer Institute. BCSC's data consist of information gathered from both private practice and academic facilities, in both urban and rural environments. Data from seven BCSC registries were used:
- San Francisco Mammography Registry, San Francisco, CA
- Group Health, Seattle, WA
- Colorado Mammography Project, Denver, CO
- Vermont Breast Cancer Surveillance System, Burlington, VT
- New Hampshire Mammography Network, Lebanon, NH
- Carolina Mammography Registry, Chapel Hill, NC
- New Mexico Mammography Project, Albuquerque, NM
Included in the study were 4.2 million mammograms performed on 1.5 million women at 196 facilities (132 urban and 64 rural) between 1998 and 2004. For each radiologist subject, the study included two to seven years of data for a stable estimate of the average annual volume of mammography exam interpretation.
The study found that the mean annual mammographic volume was 1,777.
- 57% of the radiologists interpreted 750 to 2,000 mammograms per year
- 20% interpreted fewer than 750 mammograms per year
- 23% interpreted more than 2,000 mammograms per year
- 10% interpreted more than 3,000 mammograms per year
The study also calculated mammographic interpretation volumes by location, finding that 90% of rural radiologists read less than 2,000 exams annually, compared to 70% of urban radiologists. An annual interpretation volume under 1,000 per year translated into a small difference in the provision of mammography by location. But at higher volumes, for example 2,000 mammography exams per year, Smith-Bindman and her team found that the difference in the proportion of mammograms that urban and rural radiologists read was more distinct:
In urban centers, a minimum mammography interpretation volume requirement of 2,000 per year would result in 42% of mammograms needing to be redistributed to high-volume radiologists if low-volume radiologists stopped reading mammograms.
In rural areas, a mammography interpretation volume requirement per year of 2,000 would mean that 63% of mammograms would have to be redistributed to high-volume radiologists if low-volume radiologists stopped reading mammograms.
These results led the researchers to conclude that in doubling the annual mammography interpretation requirement per year from 480 to 1,000, one-quarter of radiologists would no longer be certified at their current workload. In addition, if these radiologists stopped interpreting mammograms, the workload of remaining radiologists would increase by about a third.
But if the annual mammogram interpretation requirement were raised to a minimum of 2,000 exams, 35% of urban radiologists and 48% of rural radiologists would not interpret enough mammograms to qualify for certification; the remaining radiologists would have to increase volumes dramatically to sustain current capacity, and the effect would be most dramatic in rural areas, the group found.
Currently, radiologists interpret a mean of 39 mammograms per week, with fairly small differences between urban and rural doctors (44 and 29, respectively).
If the minimum were raised to 2,000, workload would increase to a mean of 133 per week for urban radiologists and 263 per week for rural radiologists.
The researchers also estimated the impact of raising the annual mammography interpretation volume on facilities. If a volume requirement per facility were established at 1,000 mammograms annually, daily volume would increase by about 25%, with little difference between urban and rural facilities; but if that volume were set at 2,000, the daily volume requirement would double, from about 21 to 50 in urban locations and 12 to 31 in rural areas.
The bottom line? With the increased demand for mammography that's sure to come over the next decade as the population ages, it's crucial to understand the impact a change in the volume requirement could have on patients' access to mammography exams. If physicians who serve rural communities were unable to keep their mammography certification due to an inability to meet the minimum volume interpretation requirement, patient access would be compromised, Smith-Bindman and her team concluded.
By Kate Madden Yee
AuntMinnie.com staff writer
February 14, 2008
Related Reading
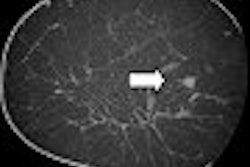
DMIST: Women under 50 with dense breasts benefit from FFDM, January 29, 2008
Even small co-pay deters mammogram use: U.S. study, January 25, 2008
Screening mammograms for elderly women encouraged, January 16, 2008
Cochrane Review studies mammo discomfort, January 25, 2008
Studies support breast CT's ability to heighten tissue contrast, resolution, January 25, 2008
Copyright © 2008 AuntMinnie.com