
Acetabular fractures are uncommon, but the prognosis is pretty dire when they do occur. Short-term complications include blood clots in the legs and pelvis, nerve injuries, and postsurgical infection. The long-term prognosis is associated with hip arthritis, osteonecrosis, and excess bone formation.
Diagnosing acetabular fracture, particularly in the trauma setting, is an elaborate process that involves multiple, time-consuming, radiation dose-heavy imaging studies. In an effort to seriously slash such a complex imaging paradigm, radiologists and orthopedists at Wake Forest University Baptist Medical Center in Winston-Salem, NC, have proposed using 3D volume-rendered CT to assess acetabular fractures. Their protocol would reduce the number of imaging studies as well as the patient dose.
In an interview with AuntMinnie.com, radiologist Dr. Craig Barnes explained that at Wake Forest "the (imaging) paradigm that is used now when a trauma patient comes in -- and this is relatively universal in the U.S. -- is a clearing lateral C-spine, an anterioposterior (AP) pelvis, and an AP chest x-ray."
"If there is significant trauma, they'll do a CT of chest/abdomen/pelvis or a CT of the abdomen/pelvis," he said. "Then if there is head injury, they'll do a CT of the head."
If an acetabular fracture is identified, the patient can look forward to more imaging, including Judet (oblique) as well as another pelvic CT, and "you end up radiating the patient two additional times," Barnes noted.
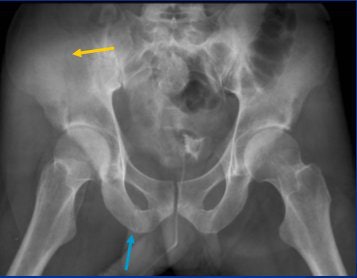 |
| AP plain-film pelvic x-ray. Fractures involving right iliac wing (yellow arrow) and obturator ring (blue ring) are difficult to see despite good-quality AP film and exposure. All images courtesy of Dr. Craig Barnes. |
At the 2007 RSNA meeting in Chicago, Barnes presented a study that his group performed on 23 patients who met the following criteria: presence of acetabular fracture, x-rays of both AP and Judet views, and thin-slice CT datasets, most of which were obtained on a 64-slice scanner (GE Healthcare, Chalfont St. Giles, U.K.).
From the CT data, a total of 69 image sets were created, consisting of plain films and either translucent 3D CT images or surface-rendered 3D CT images (TeraRecon, San Mateo, CA).
The images were then independently presented and reviewed by two radiologists and two orthopedic surgeons, who classified the pelvic images according to the Judet-Letournel system. Final classification was done in consensus by the whole group. A generalized linear model with clustered measurements was fitted to the CT data, and a correct or incorrect diagnosis was used as the response variable.
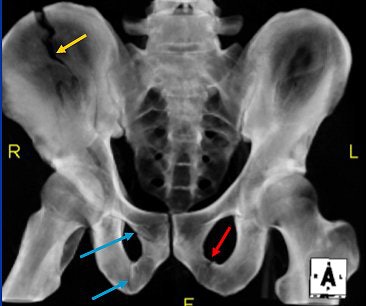 |
| Translucent 3D volume-rendered CT of AP pelvis. Fracture involving right iliac wing (yellow) and right obturator ring (blue arrows), which in combination relate to anterior column fracture. This is more easily seen on reformatted 3D image reconstructed from trauma CT. Additionally, a left inferior pubic rami fracture is seen (red arrow). |
According to the results, there was no difference between 3D volume-rendered CT images and plain-film images with respect to the accuracy of classifying acetabular fractures. Using 3D translucent reformatted views, reader accuracy came in at 73% and 71% for 3D surface-rendered reformatted views, versus 60% for the plain films.
"What we would like to suggest is that there is a potentially new diagnostic paradigm that we could use," Barnes said during his RSNA talk. "We could do an AP (x-ray of the) pelvis, CT of the chest/abdomen/pelvis or abdomen/pelvis ... then 3D reconstruction could be done from that trauma CT. This would eliminate the Judet views as well as the additional pelvic CT. With this new diagnostic paradigm, we'd have quicker patient throughput, less radiation dose, a decrease in patient discomfort, and a decrease in cost, but maintain diagnostic accuracy."
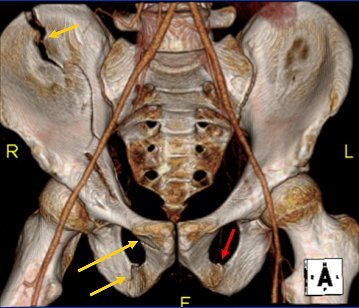 |
| Surface 3D volume-rendered CT of AP pelvis. Right anterior column fracture is well-demonstrated on reconstructed image from trauma CT. The left pubic rami fracture is more subtle than on translucent image. |
But a key to making this protocol work is to convince referring physicians that x-ray exams can be replaced with the 3D CT reconstructed information, Barnes said. In response to an RSNA attendee's question as to why 2D reconstruction wouldn't suffice in this setting, Barnes said that from a diagnostic standpoint, the orthopedists want the best anatomic visual for treatment planning.
Barnes told AuntMinnie.com that Dr. Lawrence Webb, an orthopedic surgeon and study co-author, has embraced this new paradigm.
"He no longer orders Judet views on initial assessment," Barnes stated, because the 3D rendering "improves (the orthopedic specialist's) understanding of what the problem is."
"The advantage of those volume-rendered images is that you can actually see the surface of the bone," he explained. "You can see whether the fracture goes to the surface of the bone. You can see how the pieces of bone interact, how far they are displaced, how many there are, whether you can take one plate and screw fixation. It gives (the surgeon) a better idea of the complexity of the case so that when he gets in there, there are no surprises."
Making nonimaging clinicians aware that there is a more sophisticated way to look at diagnostic imaging information can also go a long way in reducing the excessive radiation exposure that modern patients receive.
"You have to show the people who order the plain films that they don't need them," Barnes said. "I think it only makes sense that in this new world of CT and volume datasets, you want to get the most out of (imaging) and manage patients better."
By Shalmali Pal
AuntMinnie.com staff writer
December 13, 2007
Related Reading
MRI, CT prove their metal for imaging orthopedic hardware, May 4, 2007
The ABCs of MRI for hip disorders, February 2, 2007
3D penetrates trauma imaging niche, August 4, 2006
Copyright © 2007 AuntMinnie.com



















